America has immunized troops since George Washington’s time. Here’s how to improve military (and civilian) vaccination programs
By Daniel Gerstein | July 27, 2023
 John Trumbull's 1786 oil painting depicting the death of the American revolutionary general Richard Montgomery during a failed attack on the British in Quebec. Before the battle, the American forces grappled with a crippling outbreak of smallpox.
John Trumbull's 1786 oil painting depicting the death of the American revolutionary general Richard Montgomery during a failed attack on the British in Quebec. Before the battle, the American forces grappled with a crippling outbreak of smallpox.
In 1776, George Washington was facing a serious obstacle in his quest to defeat British colonial forces in America. Smallpox was crippling his army. In fact, an outbreak the prior year had probably caused a major offensive to fail. The British had more immunity to smallpox than the revolutionaries, and Washington needed to put his forces on a sounder immunological footing. Before the development of vaccines that meant turning to a procedure known as variolation—where material from a smallpox sore is scratched into the skin of healthy people or inhaled through the nose. It was safer than contracting the disease naturally, but still carried plenty of risk. Recovering patients could spread smallpox if they didn’t carefully quarantine and sometimes the process killed them outright. Though Washington had misgivings about variolation, in the end he decided to mandate it, thereby setting a precedent for inoculating troops.
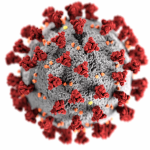
Infectious diseases have long wrought havoc on the ability of militaries to operate, and since Washington, other US leaders have also had to consider how best to protect national security interests against pathogens. Most recently, of course, defense officials grappled with the effects of the COVID-19 pandemic on military preparedness. An outbreak occurred on the USS Theodore Roosevelt, an aircraft carrier with close to 5,000 personnel on board, in March 2020, vividly illustrating this point. The Roosevelt had to be taken off mission and was ordered to Guam as COVID spread rapidly among the crew, eventually infecting more than 1,200 sailors, one of whom died. Initially, he Navy removed the captain of the Roosevelt, who had sent an email to several people that recommended the vessel be evacuated. That controversial decision ultimately forced the top Navy official, himself, to resign. This vignette serves as a poignant reminder of why the Department of Defense has a vaccination program: to ensure force health protection and mission readiness.
Today, the military requires nine immunizations for all uniformed personnel. These include measles, mumps, rubella and Hepatitis A and B, to name a few. Usually, these mandates are uncontroversial, but during the COVID pandemic, thousands of service members balked at vaccine requirements. Given how critical they are to military readiness, it’s worth considering how to make vaccination campaigns as successful as possible. To that end, my colleagues and I at the Rand Corporation have developed a framework for assessing the acceptability of future military vaccination campaigns based on lessons learned from three previous programs relating to anthrax, smallpox, and COVID-19. Using this methodology can help officials shape a program and address areas that are likely to be of concern.
The three programs. The anthrax vaccination program officially began in 1997, during the administration of former President Bill Clinton. Clinton famously had become concerned with biowarfare after reading The Cobra Event, a novel about a bioterrorist, and undertook several initiatives in response to the perceived threat, including creating a stockpile of medical countermeasures. The anthrax vaccine was to be administered over 18 months, with annual boosters thereafter. To ensure vaccine safety and efficacy, the secretary of defense established four preconditions for beginning the vaccinations, including developing a system for tracking them and having an approved operational and communications plan for the program.
Despite these efforts, when the campaign began in August 1998, there were almost immediate concerns, with one Government Accountability Office survey finding that 65 percent of the force did not support the campaign based on the “completeness, accuracy, timeliness and potential bias of the information provided.” The survey also showed that 86 percent of those vaccinated had experienced side effects or adverse reactions, though the report noted that most did not report their specific symptoms.
Almost one million service members had received anthrax vaccinations by the time a lawsuit halted the program. The 2003 suit alleged that the vaccine had not been approved for use against inhalational anthrax, which would be how troops would likely be exposed to anthrax spores in a biowarfare scenario. The judge in the case said the vaccine was an investigational drug “being used for an unapproved purpose.” Although the mandatory program ended, the Pentagon sought and won Food and Drug Administration (FDA) approval for an emergency use authorization to vaccinate high risk personnel in 2005 and the program restarted the next year. The challenges with the rollout of the vaccine contributed to concerns about its safety and efficacy and a loss of confidence in it. Based on potential in-theater risks, servicemembers still receive anthrax vaccinations prior to deployment.
While smallpox, which has a fatality rate of about 30 percent, was declared eradicated in nature by 1980, US officials harbored concerns that terrorists or adversarial countries might use the variola virus that causes it as a weapon. Unlike the military’s anthrax campaign, the 2002 smallpox program began with a carefully monitored pilot effort at four locations and with service members who had undergone screening to ensure they were unlikely to suffer adverse effects. Officials clearly communicated the results of that effort throughout the force. Military leadership highlighted the rationale for the program. And overall, government auditors declared the program a success.
contrast to the anthrax and smallpox campaigns, which applied to Defense Department personnel, the COVID-19 vaccine program was a response to a pandemic. It began as a voluntary (yet recommended) program within the Defense Department, but became mandatory after the FDA changed the status of the mRNA vaccines against COVID-19 to fully approved. Operation Warp Speed, the US government’s COVID vaccine development program, ultimately resulted in the most rapid approval of a vaccine in history, with vaccines developed and ready for distribution in less than a year. During the year that the vaccine was being developed, misinformation, disinformation, and mixed messages contributed to vaccine hesitancy, including in relation to the military vaccination program. For example, the overemphasis in the media on the novel technology behind the mRNA vaccines may have contributed to service member concerns that the vaccines were “experimental,” despite receiving full regulatory approval.
The military followed the guidance of the National Academies of Sciences, Engineering, and Medicine during the early vaccination campaign, which prioritized groups for vaccination based on factors such their risk of severe illness. However, after the FDA approved Pfizer’s COVID vaccine, the secretary of defense ordered military branches to vaccinate all members who were not already fully vaccinated against COVID-19.
While vaccination rates within the Department of Defense reached over 99 percent for uniformed personnel by December 2022, there was some resistance in the ranks, and over 8,400 servicemembers were discharged for refusing to be vaccinated.
How to assess vaccination programs. The military’s three mandatory vaccine campaigns (anthrax, smallpox and COVID-19) created an opportunity to consider the development of a successful vaccination program. My colleagues and I have identified six key attributes for consideration and establishing a mandatory vaccine policy: (1) approval status of vaccine, (2) confidence in the technology, (3) targeted groups for vaccines, (4) perceived care in making decisions about mandates, (5) consistent messaging, and (6) level of disinformation surrounding the vaccine. We identified five rating levels for each attribute, with five representing the best-case scenario.
For example, looking at the attribute of “approval status,” the most advantageous rating of “5” would be for vaccine that the FDA has fully approved. The next most advantageous rating would be for one that has received an emergency use authorization followed those that have investigational new drug status.
The average scores (out of a possible score of 5) for the six attributes of the vaccination campaigns we analyzed were: smallpox at 4.8 and anthrax and COVID-19 at 2.5.
It’s easy to see some of the reasons for the lower scores of the anthrax and COVID campaigns as compared to the smallpox program. In the case of the anthrax effort, the military was using a vaccine with an uncertain regulatory status; it had not been approved for inhalational anthrax, even though that was the envisioned threat. In the case of the COVID vaccination program, the newness of the mRNA vaccine technology arguably led some came to believe the vaccinations were experimental or not proven, creating hesitancy. The issues we identified related to the attributes of messaging, technology, and disinformation.
By analyzing where a potential vaccination campaign would score on the attributes we assess in our framework, officials could make adjustments to improve the overall acceptability of a program. This analysis highlights it is advantageous to show prudence in targeting specific groups and the decision making that goes into which groups are prioritized for vaccination. In the case of the well-received smallpox vaccination program, for example, priority was given to those involved in special missions that could be at greater risk for becoming exposed to this deadly pathogen. Consistent messaging and efforts to combat disinformation should also be prioritized in mandatory vaccine campaigns.
These attributes of military vaccination campaigns also provide an approach that should apply to a successful non-military vaccination campaign. Meeting communities where they are and taking the time to explain the rationale for vaccinations are important principles to be followed by leaders and public health authorities. This does not mean that all will be enticed to get vaccinated by these interventions, but the likelihood of gaining increased acceptance rises through community engagement and must be considered in the early stages of vaccine development as well as during the implementation of a vaccine program.
Together, we make the world safer.
The Bulletin elevates expert voices above the noise. But as an independent nonprofit organization, our operations depend on the support of readers like you. Help us continue to deliver quality journalism that holds leaders accountable. Your support of our work at any level is important. In return, we promise our coverage will be understandable, influential, vigilant, solution-oriented, and fair-minded. Together we can make a difference.
Keywords: vaccine hesitancy
Topics: Biosecurity