Rabid anti-vaxxers could help spread deadly disease
By Dawn Stover | September 12, 2023
 Photo by Karsten Winegeart/Unsplash
Photo by Karsten Winegeart/Unsplash
In mid-August 2021, an Illinois man in his 80s woke up with a bat on his neck. The bat was captured and tested positive for rabies. The man was advised that he should immediately begin post-exposure rabies treatment, a regimen that includes several doses of rabies vaccine and is virtually always effective in preventing the onset of rabies.
However, he declined treatment, according to a case report from the Illinois Department of Public Health. He was reportedly afraid of vaccines.
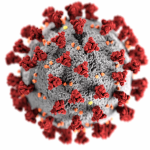
A month later, he began experiencing symptoms of rabies, a gruesome disease that attacks the central nervous system and can cause muscle spasms, headache, difficulty with speaking, irritability and aggressiveness, hallucinations, and severe swelling of the brain. Death usually comes 7-10 days after symptoms begin, and the Illinois man was not spared. Rabies has the highest mortality rate of any infectious disease in humans. Only a few people have ever survived it.
Rabies kills about 59,000 people worldwide annually, but only one or two people in the United States die of the disease in a typical year. That’s largely because of two highly successful interventions since 1960: widely available post-exposure treatment for humans and widespread preventive vaccination for dogs. In the wake of the COVID-19 pandemic, however, both of those interventions may be threatened by vaccine hesitancy—the reluctance or refusal to vaccinate despite the availability of effective vaccines.
Canine vaccine hesitancy. Vaccine hesitancy, which gained traction during the pandemic, isn’t just affecting human vaccinations. A new study reports that dog owners in the United States are also skeptical about vaccines for their pets, including vaccination to prevent rabies.
The new study, which is still in press but was published online by the journal Vaccine on August 26, reported that more than half of the 924 dog owners contacted in a nationally representative survey of 2,200 adults consider dog vaccines to be unsafe, ineffective, or unnecessary. More than a third of the dog owners surveyed believe canine vaccination can cause autism in pets. (There is no scientific evidence for autism in dogs or for a connection between autism and vaccination.)
“Troublingly, we find that [canine vaccine hesitancy] is associated with rabies non-vaccination, as well as opposition to evidence-based vaccine policies,” wrote the three authors of the Vaccine piece—an expert on public attitudes toward science, a veterinarian, and a political scientist. They also found that dog owners who endorse misinformation about the safety of human vaccines are 33 percent more likely to be classified as canine vaccine hesitant.
Most human rabies deaths are in Africa and Asia, and 99 percent of all human rabies is acquired from dog bites. In the United States, however, most people who die from rabies are infected by bats, according to the Centers for Disease Control and Prevention (CDC). Rabies can also be transmitted in the saliva of wildlife such as raccoons, skunks, and foxes—and wildlife can infect unvaccinated pets as well as humans. The CDC has proposed new restrictions on importing dogs from countries at high risk for dog rabies, after seeing a rise in fraudulent vaccination documents.

Although most US states require rabies vaccination for dogs and cats, there is little enforcement. If vaccination levels in the United States drop below 70 percent of the dog population, that could lead to rabies outbreaks in domestic dogs. The disease could then spread from dogs to humans.
In a 2022 survey, one in four veterinarians reported that some clients had raised political objections about requirements to vaccinate for rabies. The number of pet owners declining rabies vaccinations or expressing concerns about them has increased since COVID-19 vaccines became widely available.
A less-appreciated aspect of widespread vaccine hesitancy is that it could not only make humans reluctant to get their pets immunized against rabies but could also make some humans reluctant to get rabies vaccinations after a potential exposure to this deadly disease.
Human vaccine hesitancy. Even before the COVID-19 pandemic, the World Health Organization identified vaccine hesitancy as one of the top 10 threats to global health. The pandemic made that threat worse, with childhood immunizations declining in more than 100 countries.
Vaccination is one of the most cost-effective ways of preventing diseases. The World Health Organization estimates that vaccination prevents more than 3 million deaths a year from diseases including measles, flu, whooping cough, and tetanus—and expanded vaccination coverage could spare another 1.5 million lives.
So why are some people reluctant to get the jab? The reasons include complacency, inconvenience, and a lack of confidence in vaccines—which has been amplified by conspiracy theorists spreading false information about vaccine safety. For example, presidential candidate Robert F. Kennedy Jr. wrongly claimed in a recent podcast interview that “there’s no vaccine that is safe and effective.”
In a typical year, 30,000 to 60,000 Americans get post-exposure prophylaxis to prevent rabies after being in close contact with wildlife or unfamiliar animals, especially after being bitten or scratched. The treatment is a dose of human rabies immune globulin (which produces an immediate but short-lived immune response to rabies) administered on the day of exposure, along with one dose of rabies vaccine that is given at the same time and three other doses that are given over the following two weeks to produce a more sustained immune response.
Rabies is such a horrific disease that complacency and inconvenience generally don’t stop anyone from getting post-exposure prophylaxis. But dread of vaccines or doubts about their effectiveness could be obstacles for some people. That’s what made the Illinois man decline treatment, and it’s possible there will be others who likewise decide against vaccination, especially if they’ve had only a suspected exposure rather than a bite from an animal with a confirmed case of rabies.
Mandating rabies vaccination for dogs, or for humans who may have been exposed to rabies, is problematic. The Vaccine study found that owners who are hesitant about vaccinating their dogs are also more likely to oppose mandatory rabies vaccination.
Together, we make the world safer.
The Bulletin elevates expert voices above the noise. But as an independent nonprofit organization, our operations depend on the support of readers like you. Help us continue to deliver quality journalism that holds leaders accountable. Your support of our work at any level is important. In return, we promise our coverage will be understandable, influential, vigilant, solution-oriented, and fair-minded. Together we can make a difference.
Keywords: COVID-19, dogs, rabies, vaccine hesitancy
Topics: Biosecurity