Bird flu in cattle: A step closer to humans or a random event?
By Georgios Pappas | April 26, 2024
 A cattle farm. Credit: Lewis Clarke
via Wikimedia Commons. CC-BY-2.0.
A cattle farm. Credit: Lewis Clarke
via Wikimedia Commons. CC-BY-2.0.
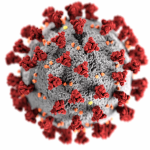
The two-year saga of rapid evolution and multi-species adaptation of H5N1 avian influenza took a drastic turn in recent weeks when the virus was detected numerous times in US cattle, raising fresh concerns that the “bird flu” virus could soon become a human threat. While cattle are susceptible to influenza viruses, until now, health officials had never detected infections with the avian strain, adding the ruminants to the increasing number of susceptible mammal species. A human case in a dairy farm worker was later confirmed, raising numerous questions about whether contact with cattle could cause infections and whether H5N1 might acquire dangerous mutations in cows.
By April 24, the US Department of Agriculture (USDA) had reported 33 herd detections of H5N1 in eight states: Idaho, Kansas, Michigan, New Mexico, North Dakota, Ohio, South Dakota and Texas. In cattle, H5N1 virus shows up in the mammary glands. Infected animals typically produce less milk. The milk looks different, too, with an appearance like colostrum, the thick, nutrient-rich yellowish milk that new mothers produce for a few days following a birth. Cattle don’t die from H5N1 infection, and the isolated human case was relatively benign. The worker’s only symptom was conjunctivitis, or pink eye. (The worker may have been infected during milking procedures that can generate infectious aerosols or through hand-to-eye contact.)
How were cows infected, and is there evidence of cow-to-cow transmission? The route of cattle herd infection remains uncertain: Cows could have become infected through grazing in H5N1-polluted environments (from remnants of birds fatally infected or from infected birds’ droppings). Reportedly, infections in pigeons, crackles, and blackbirds—peridomestic species that live around humans—preceded cattle infection in some farms. Cows may also have been infected through poultry litter used for feeding, although this litter is theoretically thermally processed before use. A similar route of infection was implicated in the domestic cat H5N1 outbreak in Poland in summer of 2023. (Using animal protein in food is a process only allowed for non-ruminants in Europe, although this policy may also be in need of revision. Pigs, which are not ruminants, are important mixing vessels for a variety of influenza viruses, which can mix and match portions of their genomes in the animals.)
Cow-to-cow infection is also a possibility, but this type of transmission was probably indirect: Since H5N1 grows in the udders of cows, there is a possibility that infectious, non-sanitized milking devices, or even the hands of dairy farm workers, were the actual means of viral transmission between the animals. As Suelee Robbe Austerman of the USDA’s National Veterinary Services Laboratory noted, there is no evidence of the virus replicating in cattle bodies outside the mammary glands. And there is no need for mass cattle culling, contrary to what happens with domestic poultry, in which infections are fatal. H5N1 infection in cows is self-resolving and not evidently directly transmissible between mammals.
The H5N1 detections in cattle coincide with the spring northbound movements of herds. It may be that there was a single spillover event that started in a herd in Texas, and then, through interstate cattle herd transport, the virus was spread to herds in other states. One has to remember, though, that Texas sits on a major migratory bird route used by hundreds of species in the spring.
Is milk a risk for humans? A recent preprint reports that cats residing in farms with infected cattle were infected (and experienced serious disease) after consuming raw milk. Human consumption of raw milk carries other infectious risks in any case, but at present it should be strictly prohibited until it is known whether these cattle H5N1 infections are a rare event or a precursor of an extended cattle-H5N1 interaction.
Is pasteurization thorough enough to alleviate the risks of H5N1 presence in the milk of infected cattle? An April 24 announcement from the US Food and Drug Administration (FDA) noted that viral particles were identified through testing in pasteurized milk samples, although the initial results from further experiments did not demonstrate the presence of “viable” infectious virus.
A previous study demonstrated that pasteurization for a period of six hours was adequate in inactivating numerous viruses in blood plasma, including an H5N1 strain, which did not behave differently from other enveloped viruses in this context. The virus would thus not be expected to demonstrate any peculiar resistance patterns to milk pasteurization, which remains an effective process of eliminating viral transmission risks. Another study focusing on chicken meat heavily infected with H5N1 showed that, at 70o Celsius, well below standard oven temperatures, 5.5 seconds of heating was sufficient to achieve a massive reduction of viral concentrations. Also, a study on avian influenza-infected eggs in the past showed that the virus was susceptible to thermal inactivation.
As the University of Guelph’s Scott Weese notes in a recent blogpost, even if infected milk enters the milk supply, milk from other sources will cause it to be rapidly diluted. Results of studies and experiments on the effect of pasteurization in H5N1-infected milk from the current outbreak could help alleviate the average consumer’s fears regarding milk.
Is cattle infection a step towards adaptation to humans? Researchers at Iowa State University investigated genetic markers in viral samples from infected cattle and demonstrated the presence of features suggesting the virus in cattle had increased affinity for receptors on human cells and increased mammalian virulence. In a preprint not yet peer reviewed, the researchers found certain point mutations that would increase the affinity that the hemagglutinin (HA) viral protein, responsible for binding to living species’ receptors, has for mammalian receptors. The influenza strain lacked, however, important traits in the key polymerase basic 2 (PB2) protein, a protein that largely regulates viral virulence. These traits are considered crucial in the pathway to human adaptation.
On the other hand, as a technical report of the Centers for Disease Control and Prevention (CDC) has demonstrated, the viral sample from the recently infected human did show such a trait, what’s called the E627K mutation, despite its absence in the sampled cattle from the same farm. The presence of the trait indicated that H5N1 adapted during human infection, although it still failed to induce a respiratory infection.
Is it therefore an accident or one more step? If there were sustained avian flu outbreaks in cattle herds, there would be an extended interface between H5N1 and humans—namely the individuals occupied in cattle farming and milk collection. Whether this increased viral-human interface can facilitate rapid viral adaptation and lead to human-to-human transmission potential (a pre-requisite for a future H5N1 pandemic) remains to be seen. The same stands for the possibility of this increased interface to lead to other viral adaptations that may lead to increased virulence to humans.
To reduce the chances of human-to-human transmission, livestock workers should use personal protective equipment (including goggles and face masks) when milking. They should sanitize equipment used in milking before using it with other animals. Further measures like restrictions in cattle movements both within and between states might become necessary if the outbreak continues.
To fully understand the extent of the cattle outbreak, however, public health and agriculture authorities should engage in extended testing and cooperate in an effort to increase awareness about H5N1’s clinical presentation in cows. Human H5N1 infections can’t be diagnosed with commercial rapid influenza tests. The only clue to such a diagnosis may be suspicion based on history and occupational exposure. Public education, therefore, on the risks to livestock workers is necessary. The USDA has released biosecurity guidance for the livestock industry.
A stock of candidate vaccines for avian influenza is available in the United States and some other countries, enough to immediately vaccinate first responders and exposed health care personnel. The H5N1 strain from the human case is extremely similar to the strains included in those candidate vaccines. But should a pandemic emerge, large-scale influenza vaccine preparation will take months using traditional manufacturing processes. (Novel vaccine platforms and approaches that might be less time-consuming have yet to succeed in bringing any influenza vaccines to the market.) Fortunately, oseltamivir, the most widely used antiviral treatment for influenza, appears to remain an appropriate and effective therapeutic option for human H5N1 cases.
In the meantime, the panzootic is expanding. Cows were not the only ruminants that recently proved susceptible to H5N1. Newborn goats on a Minnesota farm were also infected. The goats had been using the same pasture ground and water source as infected domestic poultry.
Meanwhile, by February, the panzootic had reached mainland Antarctica, where the virus infected and killed skuas, a type of predatory seabird. And investigators have been evaluating whether penguin deaths observed in the region may also be attributed to H5N1 and what the overall virulence of H5N1 is for penguins. An initial report found asymptomatic infected penguins, a sign that the infection may not be as lethal for them as for some other bird species. If it were, however, one may fear an outbreak bordering on becoming an extinction event, given that penguins live in massively populated colonies. Now, among the continents, only Oceania appears to remain unscathed by H5N1.
Finally, as underlined by a recent joint document from the European Center for Disease Control and the European Food Safety Authority, the chances of human exposure may also expand through domestic animals and particularly cats, which could potential be mixing vessel for avian and human influenza. The well-described cases in cats could simply be random events, isolated exposures that do not represent the first cases of widely circulating H5N1 in these animals. Time will tell whether the current cattle cases are also insignificant in gauging H5N1’s pandemic potential, or whether they are a step in a slow process that results in the virus adapting to and spreading widely among humans.
Together, we make the world safer.
The Bulletin elevates expert voices above the noise. But as an independent nonprofit organization, our operations depend on the support of readers like you. Help us continue to deliver quality journalism that holds leaders accountable. Your support of our work at any level is important. In return, we promise our coverage will be understandable, influential, vigilant, solution-oriented, and fair-minded. Together we can make a difference.
Keywords: H5N1
Topics: Biosecurity