TB studies illustrate the importance of properly assessing the risks of pathogen research
By Anurag Agrawal | May 28, 2024
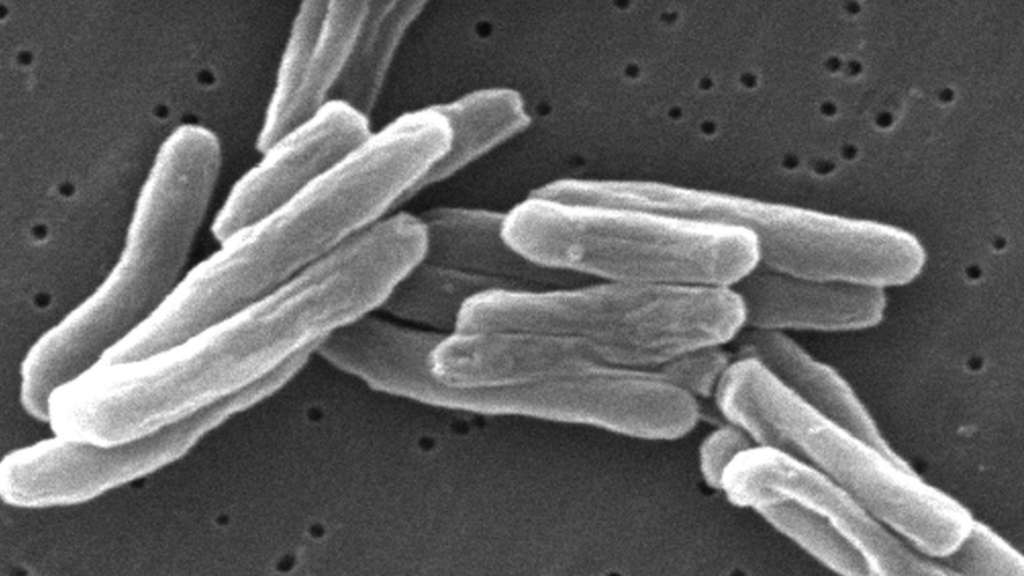 The tuberculosis bacterium, M. tuberculosis. Credit: CDC.
The tuberculosis bacterium, M. tuberculosis. Credit: CDC.
Editor’s note: This article is part of a collection of expert commentaries. You can read the rest of the series here.
It is true that the next pandemic is a matter of “when,” not “if.” The statistical certainty of a future pandemic has led to increasing research into potential pandemic pathogens so that we may create lifesaving countermeasures. Such research, unfortunately, also carries a risk of bringing about exactly what it seeks to prevent. Human error or even deliberate action is as likely to be the cause of the next pandemic as natural origin. Such concerns have intensified after the COVID-19 pandemic, which a significant percentage of the US population, at least, believes began with a research accident, one of the two main pandemic origin theories, with the other being the jump of a virus from animals to people. The question then for governments and the research community is how to build confidence in the valuable work that scientists do through appropriate regulation.
While research with favorable risk-benefit profiles must be facilitated, high-risk research of either limited benefits or benefits for only a limited few must be seen through a different regulatory lens.
The heart of the matter is honest, transparent, and thorough risk-assessment, preferably from within the research community, that creates a research environment that fosters public trust. While the institutional biosafety committees maintained by research organizations review and approve pathogen research, their function is essentially to prescribe appropriate biosafety levels for proposed research, as opposed to determining whether the benefit outweighs the risk. To draw such a line, there must be clear guidance that can be consistently followed by such committees. Further, the decision-making must be transparently recorded and made accessible for external oversight, rather than what happens in the current, fragmented, opaque system, which keeps such information within individual institutions.
A revamped risk assessment would guide a regulatory system in a manner akin to how traffic lights direct traffic, where some research is deemed too risky to do (red-signal), some cleared with advice for caution (yellow-signal) via establishment of risk-management guardrails or oversight speed bumps, and a green-signal to valuable research with minimal risks. While governments have an important role to play in such regulatory enforcement, the research community should immediately take the lead in terms of providing advice or feedback regarding appropriate evaluation frameworks and regulatory emphasis. Failure to cooperatively develop effective systems in a timely manner may lead to the emergence of heavy-handed bureaucracy that impedes all pathogen research. This would be a tragedy.
Research on naturally circulating pathogens, without introducing changes, creates no new risk to humanity and should not be impeded. But it is important to be alert to research that has the potential to create new superbug versions of such pathogens. To illustrate, tuberculosis (TB) is already a pandemic with about a quarter of the global population being latently infected, of whom about 10 percent will develop active disease in the future. Extreme or total resistance to the drugs used to treat TB is on the rise, raising the specter of a fresh pandemic wave. A fitter, more virulent, and highly transmissible drug-resistant variant would be a public health nightmare. For tuberculosis research, the possibility that a more dangerous version of TB might emerge raises regulatory challenges that also apply to other pathogens with pandemic potential, with an even greater need to ensure that ongoing essential research is not affected.
First, we must be careful to not overregulate TB research to the point that the field starts shrinking at a time when the need for research is high. Lab biosafety guidelines are thus primarily kept as biosafety level (BSL)-2 plus, although BSL-3 practices are recommended for specific activities that increase personal risk. On the other hand, this should also not be seen as a free pass.
Research activities on drug resistant strains, especially protocols involving aerosolization of infectious materials, should only be undertaken if absolutely necessary, with all due biosafety guardrails. Further, even scientifically meaningful functional research, such as introduction of mutations to investigate loss of fitness or virulence in resistant strains, should face extreme scrutiny because of the potential to create a TB superbug by mistake. If at all permitted, such work should be transparently done under strict oversight.
Unfortunately, TB research is underfunded and corners get cut on biosafety while pursuing the next big idea. A renewed commitment to adequately appreciating the risks of some pathogen research would reduce the chances of this happening. In the end, pathogen research is conducted for public health benefit. Doing this work should not become the undoing of a century of gains.
Together, we make the world safer.
The Bulletin elevates expert voices above the noise. But as an independent nonprofit organization, our operations depend on the support of readers like you. Help us continue to deliver quality journalism that holds leaders accountable. Your support of our work at any level is important. In return, we promise our coverage will be understandable, influential, vigilant, solution-oriented, and fair-minded. Together we can make a difference.
Keywords: Pathogens Commentary
Topics: Biosecurity