A new mpox variant is taking off in Africa. The WHO plan for stopping it isn’t realistic.
By Georgios Pappas | August 26, 2024
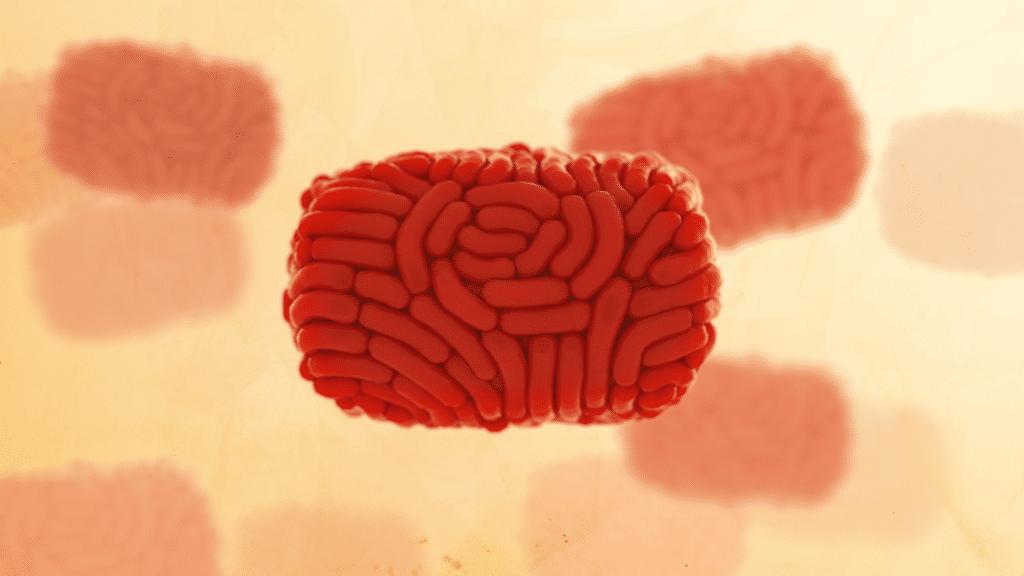 An illustration of the mpox virus. Credit: Stephanie Rossow via CDC Public Health Image Library.
An illustration of the mpox virus. Credit: Stephanie Rossow via CDC Public Health Image Library.
Beginning in the spring of 2022, mpox (formerly monkeypox) began spreading around the globe in countries outside of Africa that had rarely seen cases in the past. The mpox virus involved has infected nearly 100,000 people in two years. Though the outbreak virus caused serious symptoms, the low death rate (about 200 people have died), stands in contrast to the toll mpox had been exacting in Central Africa for years, where as many as 10 percent of the infected might die. But now a novel strain of the virus is spreading in the Democratic Republic of the Congo and other African countries and at least one case, that of an infected returning traveler, has been reported in Sweden.
The current outbreak began in the fall of 2023, when a wave of mpox cases struck Kamituga, a town in the South Kivu province of the Democratic Republic of the Congo that had been mpox-free. The most affected group were sex workers, who were numerous in the mining epicenter. And the first cases were close to the city of Bukavu, located near the country’s borders with Rwanda and Burundi—a prime location for mpox to spread in other countries. And spread it has.
The natural history of the virus in Central Africa changed.
Mpox went from being a rural zoonotic disease with secondary limited human-to-human transmission in family settings to one primarily spread from person to person, present in urban centers, and positioned to rapidly spread to other regions and countries.
But will the new version of mpox cascade around the globe again? Will it be as severe as it has been in some African countries? And is the world doing enough to deal with the outbreak in Africa? These questions and others are worth considering: The World Health Organization (WHO) has rung the alarm bell that another mpox crises may be developing.
The World Health Organization is concerned about a second mpox emergency in two years. Why? There are two main strains, or clades, of mpox. Until 2022, neither was frequently reported outside of a handful of African countries. But that changed when the Clade IIb, a virus causing a “milder” version of mpox, spread from Nigeria to Europe and elsewhere, igniting global concern and a large-scale effort to produce vaccines and immunize newly at-risk populations. Although interventions eventually brought the international Clade IIb outbreak under control, mpox continued to circulate, including Clade I, the more virulent strain endemic in Democratic Republic of the Congo.
Last week, the WHO declared an emergency involving the more lethal Clade I for two reasons: the increased dissemination of Clade I cases in Africa, even in areas and countries where it had never been detected before, and the appearance of a novel subtype of the clade called Ib. Clade Ib possesses genotypic and epidemiologic characteristics favoring human-to-human transmission.
What’s the difference between the two mpox varieties? Historically Clade II, was found in West Africa, not Central Africa like Clade I. Clade II is considered the more benign of the strains, while Clade I has caused case clusters with significant (and predominantly pediatric) mortality, sometimes with rates reaching 10 percent. Animal models suggest that Clade I virulence is indeed more significant that Clade II virulence. And that appears to be particularly true with respect to Clade IIb, the virus responsible for the 2022-2023 global outbreak, during which infections were rarely fatal.
Until 2022, the most studied outbreak of mpox outside of Africa involved the importation of Clade II-infected rodents from Ghana to the United States. The virus subsequently spread animal-to-animal among pet prairie dogs housed with the Ghanaian rodents before finally leaping from prairie dogs to their new owners. That limited outbreak belied the explosive potential of mpox. In 2022, the mainly sexually transmitted Clade IIb strain spread rapidly in non-endemic countries through networks of close contacts.
A rapid response that involved activists sharing information, contact tracing, and vaccination brought the outbreak under control; WHO ended the state of Public Health Emergency of International Concern (PHEIC) in May 2023. Clade IIb is still circulating at low levels, however. In Europe, 100 cases were diagnosed in the four-week period that ended July 4.
What is alarming about the situation with Clade I in Africa? According to the latest information from the Africa Centers for Disease Control and Prevention (Africa CDC), there has been an alarming increase in mpox Clade I cases in 2024, one that continues the trend of increased cases first observed in 2023. Cases are up 160 percent in 2024 compared to the same period in 2023, and deaths are up 19 percent. The Democratic Republic of the Congo (DRC), which has seen the brunt of the outbreak, reported 17,794 confirmed and suspected cases in 2024, with 535 deaths. It’s still unclear whether these deaths are a result of Clade Ib, or the older Clade I virus, although Clade Ib was first identified in the country.
And mpox has been moving into areas where it hasn’t been seen before. Burundi, in East Africa, has recorded its first cases, with a rapid escalation in recent weeks to 399. Authorities have also detected mpox in Rwanda, Kenya, and Uganda for the first time. Each of these countries has confirmed the new Clade Ib strain. The Central African Republic has reported 263 cases in 2024, and Congo 169 cases. Both countries have dealt with mpox before. During the past week, 1,200 cases and 24 deaths were reported from Africa (a few of the cases, but not deaths, were recorded in Nigeria, in West Africa, where the more benign Clade II has been circulating since 2022.).
The majority of cases and the vast majority of deaths from Clade I have been recorded in children. Children accounted for 66 percent of cases and 82 percent of deaths, according to the latest Africa CDC update. In Burundi, where Clade Ib has been reported, 38 percent of cases are among children under five. While a Nature article on the initial South Kivu outbreak that identified Clade Ib for the first time found it mainly affecting adolescents and young adults, including sex workers, historically, mpox in the Democratic Republic of the Congo has affected children, and the new strain seems to be amply capable of spreading among them.
So far mpox isn’t killing people at the same rate as it has in the past. Historically, mpox Clade I is thought to have a 10 percent mortality rate. Reports show the new subtype, Clade Ib, has a 3.2 percent mortality rate. That’s still high, of course, and may reflect health disparities and challenges as well as characteristics of the virus.
Will Clade Ib be able to induce a pandemic? The Clade Ib detection in Sweden will not be the last case spotted outside of Central Africa. A subtype that can readily transmit between humans will create transmission chains if given the opportunity, just as happened with the less virulent Clade IIb beginning in 2022. One silver lining, however, is that the Clade Ib virus will need sustained transmission in order to develop an animal reservoir outside the African continent, which would give it the ability to “refuel” human outbreaks—historically infections have been the result of animal to human transmission. Scientists have so far not seen that happen with the milder Clade IIb virus, for example.
But the two clades that have been causing outbreaks in recent years—first Clade IIb and now Clade Ib—have shown human-to-human transmission. To get infected, one must be in close physical contact (including sexual) with an individual with mpox. We still don’t know whether pre-symptomatic transmission occurs.
Mpox can be airborne, too—although not in the range of SARS-CoV-2, the COVID virus. Whereas with COVID, microscopic infectious particles can linger in the air and infect others who subsequently enter the same space, airborne transmission of mpox seems only possible through protracted close contact, possibly through larger respiratory droplets and less through aerosols. One review in The Lancet showed that the few symptomatic people who boarded planes or trains for long trips didn’t infect other travelers. Mpox, though, can also be transmitted by aerosolization of particles on contaminated surfaces, since viral survival in the environment can be protracted. On the other hand, we still don’t know how transmissible the novel Clade Ib subtype—described only recently—is.
But we do have a vaccine and treatments, right? A third generation Orthopoxvirus vaccine, Jynneos, developed by Bavarian Nordic initially for smallpox preparedness, was used extensively during the 2022-2023 Clade IIb surge. It has been shown to be safe for use, even for immunocompromised patients who were excluded from older vaccine generations.
Nevertheless, it is important to remember that vaccination is approved for adults. But in Africa, mpox is predominantly an infection of children, and children comprise most deaths. Vaccination may have limited effect, even if implemented extensively; one will have to hope that by vaccinating adults, chains of transmission reaching children in households will be halted. This is why, donating vaccines for adults, for a predominantly pediatric plague, as European countries have done, seems more symbolic than practically useful.
There is also no vaccine abundance. Bavarian Nordic has stated that it can speed up production up to 2 million doses by the end of 2024, with another 8 million potentially available by the end of 2025. But one has to remember that this vaccine is also a potential smallpox vaccine, and contracts existing even before the 2022 outbreak for preparedness stockpiling may interfere with the availability of the vaccine for current mpox needs.
On the therapy front, a drug called tecovirimat was developed as an antiviral for smallpox and orthopoxviruses like mpox in general. Clinical trials have been lacking, but a worrying US Centers for Disease Control and Prevention press release a few days ago stressed that despite the drug’s excellent safety profile, a clinical trial in the Democratic Republic of the Congo did not show any positive effect in Clade I infections.
What is the international community doing about mpox? In the mpox-affected areas of the Democratic Republic of the Congo and the Central African Republic, local health care systems may lack in capabilities to deal with threats like mpox. At the same time, political instability can be a barrier to improving health care facilities. Furthermore, malnutrition in the region predisposes children to unfavorable mpox outcomes. The WHO’s declaration of Public Health Emergency of International Concern (PHEIC), the designation the body gives to the most threatening crises, should have served as a chance to support this lacking health infrastructure. But the proposals so far to address the crisis don’t appear to be rising to the occasion.
The International Health Regulations Emergency Committee, a WHO advisory body, suggested that affected African countries should increase their diagnostic and surveillance capabilities, improve care for patients, including through the development of isolation care centers, and make efforts to reduce gaps in research. But the recommendations say nothing about how these targets can be achieved in countries with inadequate health care infrastructure and social unrest that has in the recent past resulted in mortal attacks against health practitioners.
The developed world is asking too much from these countries after having consistently ignored, all along, the mpox threat in them—especially the threat to children suffering from malnutrition who are without access to appropriate health care. Likewise, the announcement, by the European Commission that 215,000 adult vaccine doses for a disease mainly affecting children will be donated to these countries is mostly a symbolic gesture. One might think that the international community and WHO will probably scale up their support. But in the meantime, the African mpox epidemic might continue unabated.
Anne Rimoin, one of the world’s leading experts on mpox, recently posted online, “an infection anywhere is potentially an infection everywhere.” Declaring a Public Health Emergency of International Concern only when the risk becomes tangible for the developed countries, as the WHO has done, and issuing recommendations that essentially demand things from the mpox-stricken countries instead of outlining in detail how international help will support them, isn’t the way forward in a public health emergency. It’s the way toward further mpox spread.
Together, we make the world safer.
The Bulletin elevates expert voices above the noise. But as an independent nonprofit organization, our operations depend on the support of readers like you. Help us continue to deliver quality journalism that holds leaders accountable. Your support of our work at any level is important. In return, we promise our coverage will be understandable, influential, vigilant, solution-oriented, and fair-minded. Together we can make a difference.
Keywords: WHO, mpox
Topics: Biosecurity