Pandemic failure or convenient scapegoat: How did WHO get here?
By Thomas Gaulkin, July 9, 2020 • PDF version
On April 7, the number of reported deaths in the United States due to COVID-19 reached 12,757—surpassing the CDC’s median estimate of 12,469 deaths from the 2009 Swine Flu pandemic, during Barack Obama’s administration.
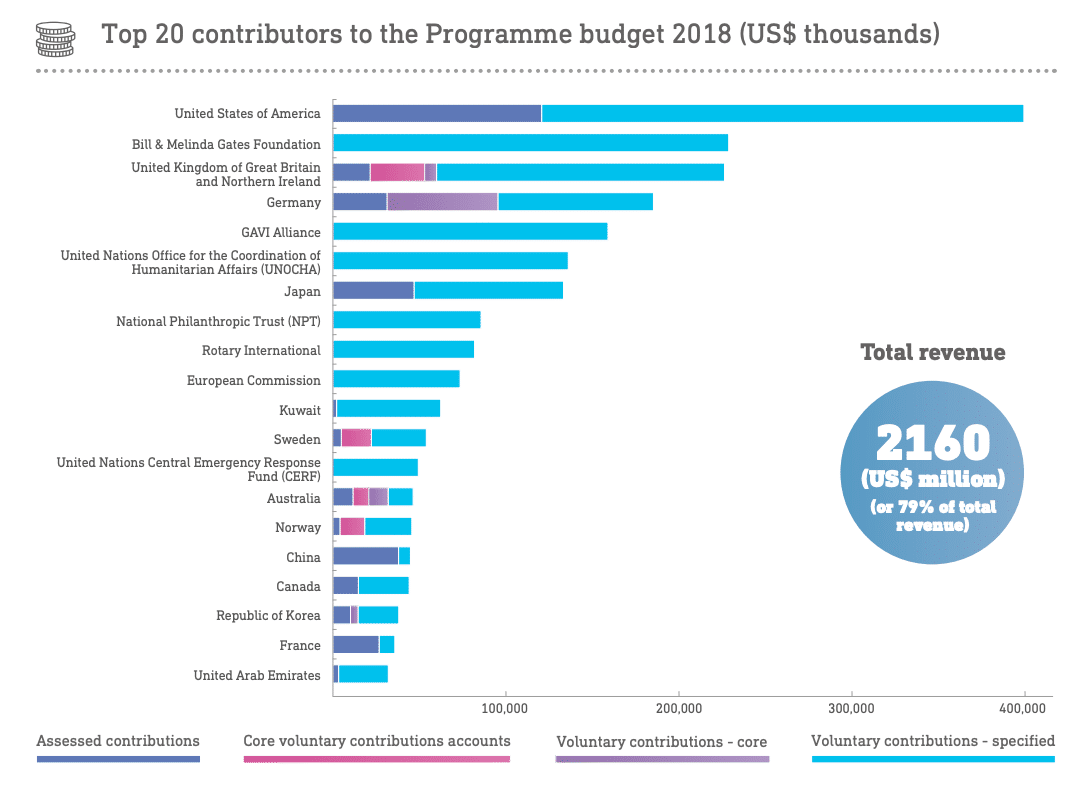
That same day, the US president began attacking the World Health Organization for failing to contain the coronavirus pandemic.
A week later, Trump declared a freeze on US funding for WHO, pending a White House investigation into its handling of the outbreak. On May 18—as COVID-19 deaths in the United States neared 100,000—the president addressed a letter to WHO’s director general, Tedros Adhanom Ghebreyesus. It included a four-page-long bullet list of complaints and closed with an ultimatum: “Commit to major substantive improvements within the next 30 days” or the funding freeze will become permanent. Trump didn’t wait that long. On May 29, he announced the United States was “terminating” its relationship with WHO and “redirecting those funds to other worldwide and deserving urgent global public health needs. The world needs answers from China on the virus.” On July 7, the Trump administration formally notified the UN that the United States would withdraw from the WHO.
But Trump is not alone in raising questions about WHO’s response to the novel coronavirus. The organization’s governing body, the World Health Assembly, passed a resolution on COVID-19 in May requiring an “evaluation” of WHO’s performance “at the earliest appropriate moment.” A preliminary report released in mid-May by the WHO Health Emergencies Programme Independent Oversight and Advisory Committee noted that while the programme had demonstrated its effectiveness by responding to 174 “acute events” worldwide in May alone, the COVID-19 pandemic “has tested WHO as never before,” particularly in the implementation of the International Health Regulations that define how the organization and its member states should respond to outbreaks.
Other WHO members and leading biosecurity experts have called for a more thorough and immediate forensic investigation of the pandemic’s origins. WHO officials have said such an investigation (which would require access to Chinese sites and records) would be dangerous at this time. “It’s like basically taking the fire engines away from the fire, and asking it to go for routine maintenance when desperately needed to put out a flame,” the WHO Director-General’s special envoy on COVID-19, David Nabarro, told CBS news.
WHO announced on July 7 that it will send a team of experts to China to begin preparations for a mission to identify how the novel coronavirus made the jump to humans—but did not specify a time frame for that mission. No matter when an independent forensic investigation gets underway (if that ever happens), the questions of how the pandemic began and why it wasn’t quashed in infancy may take years to answer. Still, it’s already clear that the developed world—with all of its advanced medical and communications technologies and national and international governance structures—undeniably and miserably failed to stop a lethal disease from infecting the globe and exacting enormous human and financial costs.
WHO had the job of being the world’s alarm system for the coronavirus outbreak. But WHO was established as and remains an organization whose members are sovereign nations; its ability to act directly when diseases threaten is limited by its members’ willingness or unwillingness to cooperate—and, more fundamentally, by the mandate and resources for intervention that its member states authorize. What does it actually mean, then, when the most powerful of WHO members, the United States of America, sternly turns around and points the finger of blame at WHO—and, in no small regard, at itself?
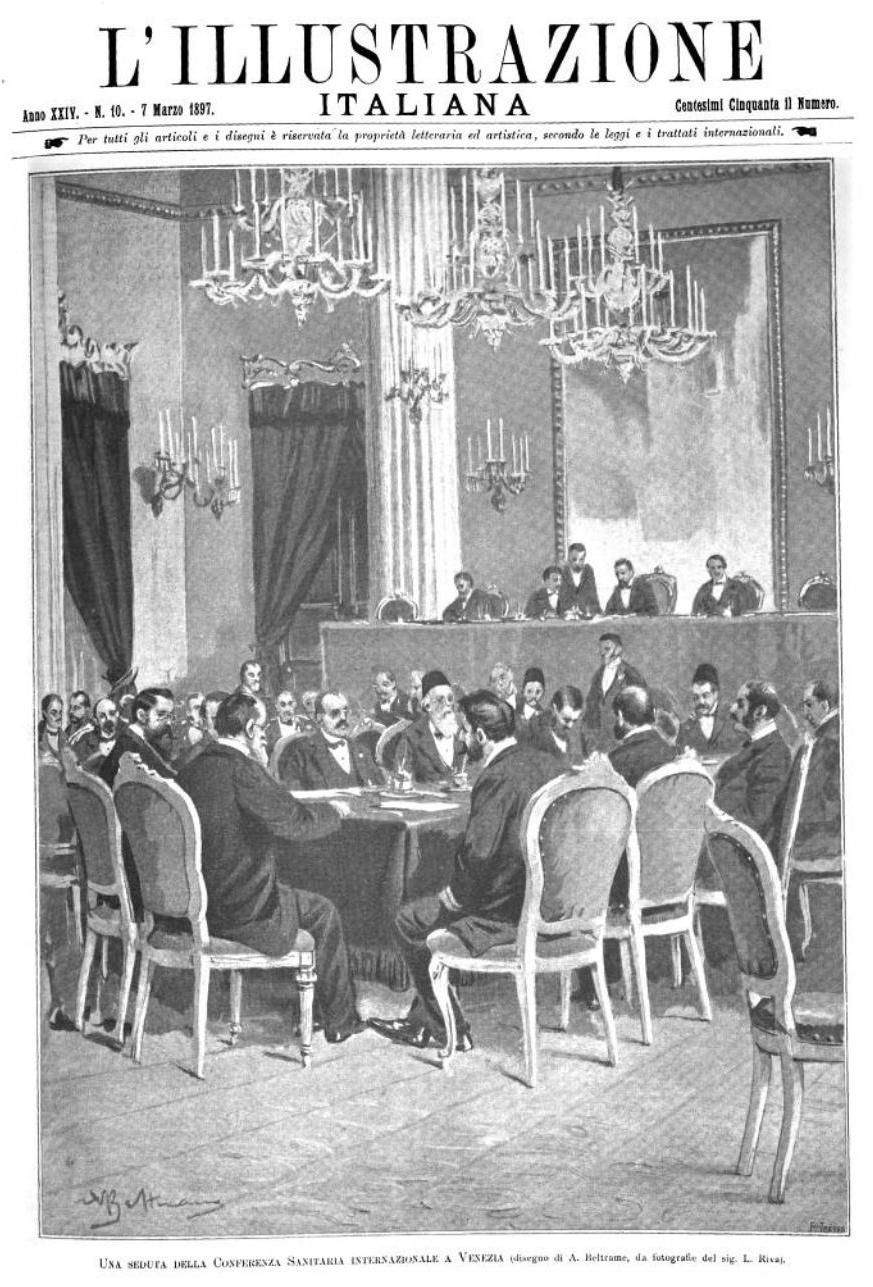
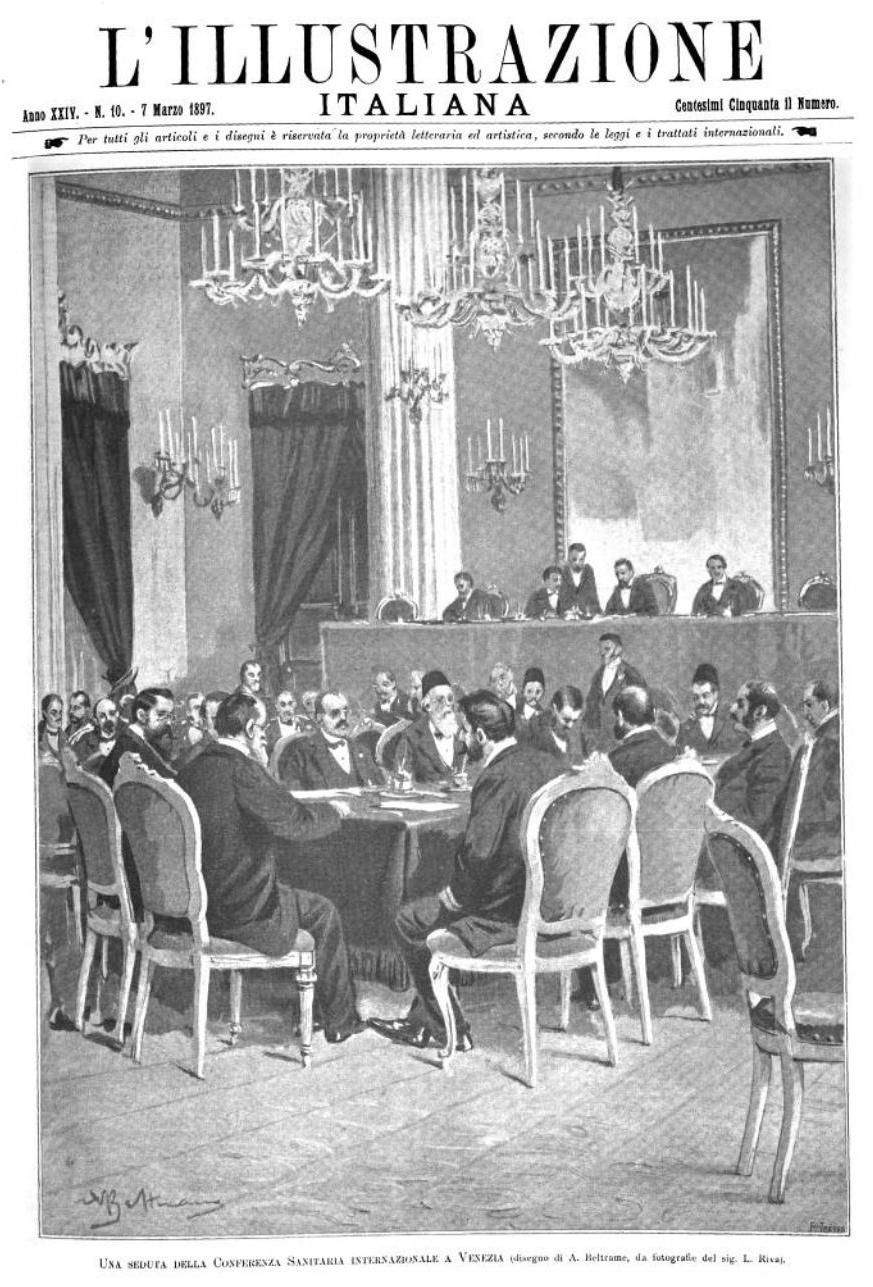
The origins of international health regulation
The earliest modern attempts to coordinate international responses to disease also reflected the specific interests of the most influential countries. Beginning in the 19th-century, concerns about the impact of disease (particularly cholera) on travel and trade led to multilateral negotiation of the International Sanitary Conventions. First proposed in 1851 and supplemented periodically until 1938, the conventions initially embodied the efforts of a small group of (mainly European) states to simplify onerous and country-specific quarantine rules (see sidebar below) that kept their trading ships literally at bay. The rules targeted a specific set of diseases—mainly cholera, yellow fever, and plague—to prevent them from reaching European borders from the east and disrupting trade.
“It was not cooperation in the spirit of finding global solutions to global problems,” University of Freiburg historian Thomas Zimmer told the Bulletin. “The spirit was ‘we need to protect our own borders.’”
From The scientific background of the International Sanitary Conferences, 1851-1938 by Norman Howard-Jones, Former Director, Division of Editorial and Reference Services, WHO.
It is of interest to cite some of the procedures that were in force, as described by Papon in 1800. On disembarking, the Master of an infected or suspected ship was required to stand before an iron grille, swear on oath to tell the truth, and then throw the ship's bill of health into a basin of vinegar. An official would then plunge the bill beneath the surface with the aid of iron tongs and, when it was judged to have been well soaked, remove it by the same means, lay it on the end of a plank, and thus present it to the ‘conservateur de la santé,’ who would read it without touching it. Letters from the unfortunate sick or suspect passengers confined to a lazaret (quarantine station) had to be thrown for a distance of ten paces, retrieved with long tongs, plunged into vinegar, and then passed through the flame and smoke of ignited gunpowder.”
Very similar precautions were prescribed in regulations promulgated in 1835 by the French Minister of Commerce. Article 614 stated that where there was need for surgical intervention, a surgical student should be "invited" to be incarcerated with the patient—students presumably being more expendable than doctors. […]
Another article (616) provided that a surgeon clad in oilskin garments could operate with special long-handled instruments provided that he carried with him a brazier for burning aromatic herbs. It was firmly believed that low spirits predisposed to epidemic diseases, and Papon cites with apparent approbation the case of a doctor who was "very careful" to drink a few glasses of wine from time to time when attending a potentially dangerous patient. "He did not get drunk," says Papon, "but he became merry." For the involuntary inmate of a lazaret, the visit of a half-tipsy doctor clad from head to foot in oilskins and bearing long-handled instruments and a portable brazier was probably less than reassuring.
But diplomatic coordination around the International Sanitary Conventions paved the way for the World Health Organization, as the first international health organizations emerged in part to provide a permanent venue for implementing the conventions. The Pan American Sanitary Bureau—which, as the Pan American Health Organization (PAHO) now doubles as the WHO’s regional office for the Americas—was established in 1903 to ease trade between the United States and Latin America; the Paris-based Office International d’Hygiene Publique was driven by European interests at its creation in 1907, but eventually took over as the global steward of the International Sanitary Conventions. One of the more successful activities of the ill-fated League of Nations was its Health Organization, which coordinated sharing of national health information, research, and prevention of disease, and set the stage for the creation of the WHO.
#Throwback to 1902 when 11 countries met in Washington D.C. to form PAHO, then called the International Sanitary Bureau! #PAHOHistory #TBT pic.twitter.com/FSolStsv5L
— PAHO/WHO (@pahowho) August 9, 2018
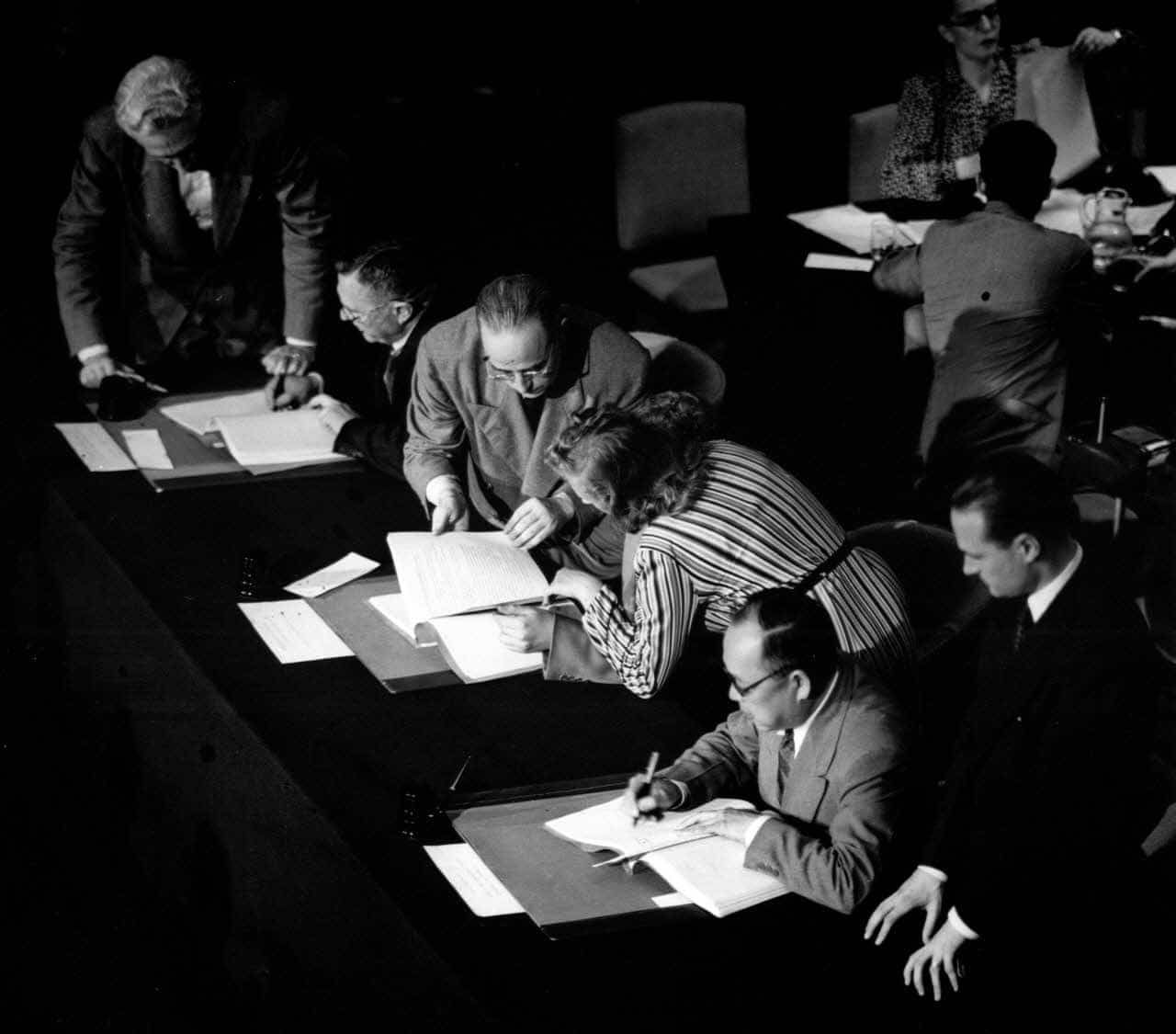
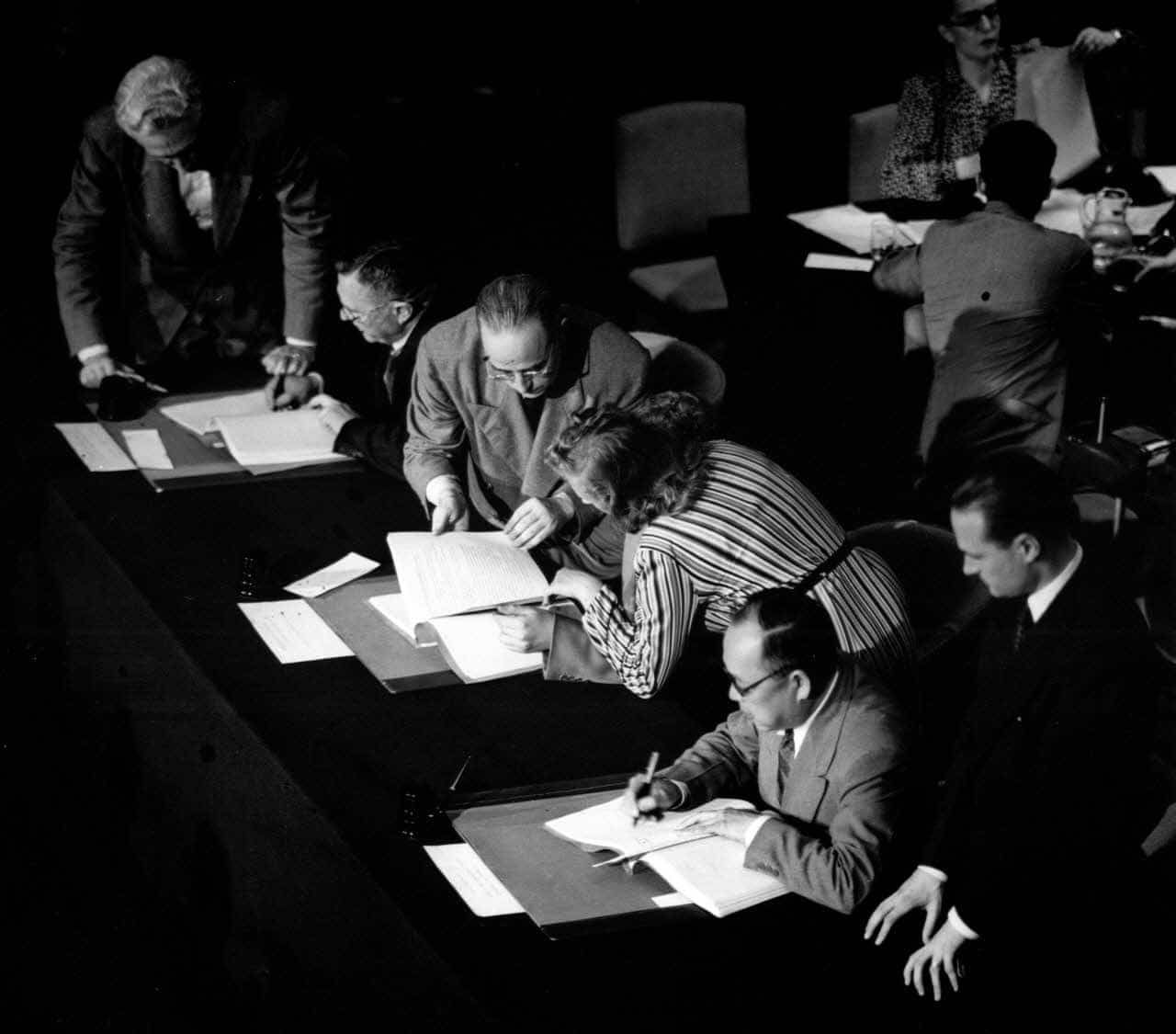
Both the Paris Office and League of Nations health operations were folded into WHO at its founding in 1948, and the WHA voted to consolidate the 13 separate conventions as a single set of International Sanitary Regulations in 1951. Revised and renamed in 1969 as the International Health Regulations, they continued to pertain only to a short list of epidemic diseases—like cholera, yellow fever, plague, and smallpox (eradicated by the late 1970s in one of WHO’s least-disputed triumphs)—through the turn of the millennium.
It took nearly five decades for the international regulations to be revised to more comprehensively address the planet’s vulnerability to contagious diseases—including influenza and coronavirus, the two viruses that have caused the deadliest pandemic outbreaks of the past century.
The Magna Carta of health
The World Health Organization was conceived in the wake of World War II “to promote and protect the health of all peoples” amid a wave of idealism about the role international institutions could play in creating a peaceful planet. The United States played a pivotal role: Then-US surgeon general Thomas Parran presided over the 1946 International Health Conference that drafted the WHO constitution. He dubbed it the “magna carta of health.”
One defining feature of the WHO constitution that distinguishes it from other specialized agencies under the United Nations umbrella is the World Health Assembly (WHA). The WHA decides the organization’s priorities and has unusually strong authority within the UN system to pass regulations and conventions that are formally binding on member states. At its founding, WHO had 55 members. Today 194 countries and two territories are represented in the WHA.
The prospect of relinquishing any form of sovereign control to a UN body has always been controversial in the United States. Although President Truman quickly approved US membership in WHO in 1946, legislators delayed ratifying the WHO constitution until just 10 days before the first World Health Assembly convened in June 1948. Some in Congress argued that WHO would be “an agent of socialized medicine, that the WHO was too close to the Soviet Union,” Zimmer said.
In fact, just a year after WHO’s founding, the Soviet Union was the first member state to withdraw its membership. Though it rejoined in 1956 during the so-called Khrushchev Thaw after Stalin’s death, Zimmer says the Soviet Union’s absence during the early years opened room for US interests to dominate the organization’s agenda.
“For most of [WHO’s] existence, it’s been shaped to a significant degree by whatever the United States would allow it to be, or would not allow it to be,” Zimmer said. “That should be reflected in our thinking about what we can expect from this institution.”
Catching the flu early on
The United States was an early contributor to WHO’s work to prevent pandemics, particularly with influenza. The Global Influenza Programme was among the first projects developed by WHO, proposed even before WHO’s constitution took effect. At first consisting of a single World Influenza Center based in London, the program soon added a collaborating center in the United States. These early collaborations were formalized in 1952 as the Global Influenza Surveillance Network. The network today has six collaborating centers, 144 National Influenza Centers, and additional labs in 122 countries devoted to surveilling viruses, gathering samples, and sharing data to enable speedy response to outbreaks and vaccine development.
“There are no laboratories at the WHO headquarters in Geneva,” said Nancy Cox, former head of the US Center for Disease Control and Prevention’s influenza program. “All of the laboratory work and epidemiology work as well is done in-country. Data are collated and sent to the World Health Organization, where they try to put together a global picture for influenza.”
(Even though COVID-19 is caused by coronavirus, Cox told the Bulletin, “there's been a long-term recognition of the fact that an influenza pandemic plan can be rapidly repurposed for another respiratory pathogen. An influenza surveillance system can be rapidly repurposed for a new pandemic threat.”)
The global picture during the first pandemic events on WHO’s watch was quite different from today. Although the United States suffered 116,000 fatalities from the 1957 “Asian flu,” which killed up to four million worldwide, that pandemic and the later 1968 “Hong Kong” influenza, which killed around one million people globally had little impact on WHO’s agenda. At the time, vaccines had proven their worth against seasonal flu and other diseases. WHO’s priority at the time was global eradication of malaria—encouraged by the invention of DDT and heavily sponsored by the United States, which sought to open up economies of developing nations during the Cold War. The public perception was that it was just a matter of time before science would eliminate malaria and other epidemic threats. “This was a period when the belief in biomedical technical solutions to treat infectious disease was still very strong,” Zimmer said.
“It’s honestly striking how small the cultural footprint was,” Zimmer said. “When you have this really aggressive flu pandemic spreading around the world, killing almost 120,000 Americans, there was no one saying, ‘Oh, my god, is this the new Spanish flu? Is this the new global pandemic?’ It was just like, ‘Yeah, there’s a bad flu. All right, let’s get vaccinated.’”
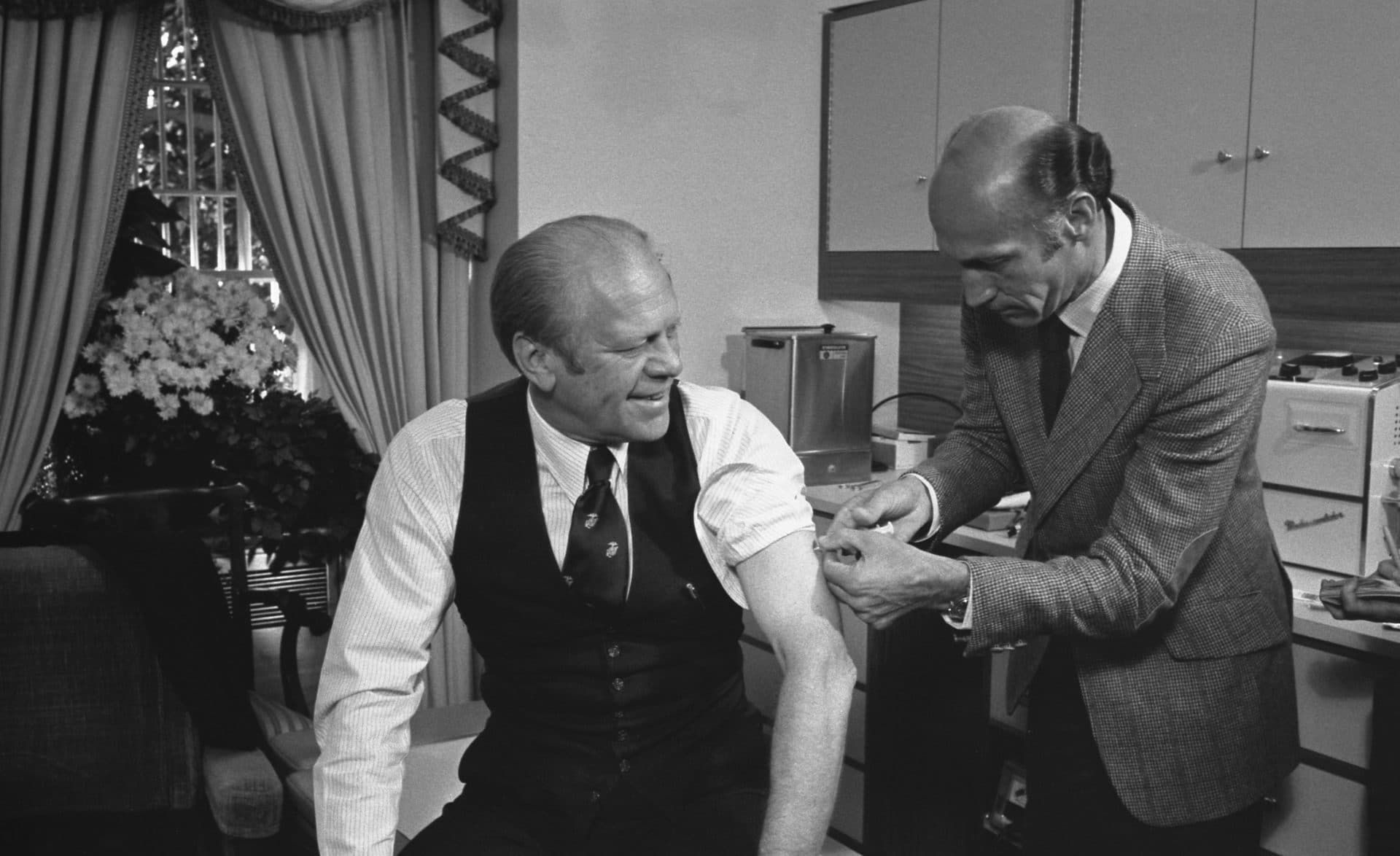
Despite the rapid emergence of new diseases in the 1970s—like Marburg and Lassa fevers, and the first Ebola outbreak in 1976—global attention to pandemics remained scant. In 1976, an epidemic of H1N1 linked to the Spanish Flu strain sparked fears about a repeat of 1918 in the United States and led to a nationwide vaccination program. But the flu’s impact turned out to be relatively mild, and the program was halted after some 45 million citizens were vaccinated, including several hundred who developed neurological disorders as a result. The “fiasco,” as the New York Times referred to it, also damaged public views of vaccines and infectious disease more broadly.
“It was seen as a complete overreaction,” Zimmer said, “as a drastic failure of both political leadership and expert leadership… As a confirmation that there was nothing much to be worried about influenza pandemics.”
Mixed agendas and budget cuts
WHO’s structure and funding went through some big changes in the 1970s and 1980s. Until then, the US was the heavy-weight driving WHO’s agenda, especially around disease eradication efforts like the malaria program. Through the decolonization process and the introduction of newly recognized independent states, WHO grew in the 1960s by nearly three dozen members from Africa alone. This new voting bloc of less wealthy states had equal votes in the World Health Assembly and sought to redirect WHO’s energies toward areas of less immediate concern to the wealthy states, like improving local health infrastructure and securing equitable access to medicine.
“[WHO] started getting involved in the regulation of the medical and pharmaceutical industry in the late 1970s,” Zimmer said. “That did not go well with the United States, and it really led to a very strange relationship between Washington and Geneva. It escalated to the point of open hostility in the mid-1980s.”
Inter-agency conflict in the UN system and the competing agendas of wealthy and developing countries helped further erode WHO’s stature. “It’s really a terribly difficult situation to manage,” Cox said. “The interests of [wealthy] countries and those of low- and middle-income countries, in terms of what health priorities should be focused on, are quite different.”
US President Ronald Reagan froze WHO’s funding in the early 1980s over these disputes, as well as emerging objections to international aid for family-planning campaigns that included abortion. Though the United States eventually resumed its funding for the organization, it has frequently remained in arrears, as it often does across the United Nations system. Three months before Trump announced a freeze, the US already owed more than $200 million of its 2020 and prior year assessed contributions (those that WHO has discretion to budget as needed for its core operations and planning).
Critically, the Reagan administration and other major member state contributors pushed a “zero-growth” policy for WHO’s regular budget, which eventually froze states’ mandatory dues to the organization at nominal 1990s levels. (The US assessed contribution 25 years ago was $104 million. In 2020 it was $120 million.) The budgetary vacuum created by this policy left the door open for increased “extra-budgetary” funding, supported entirely by voluntary contributions from member state donors and private organizations.
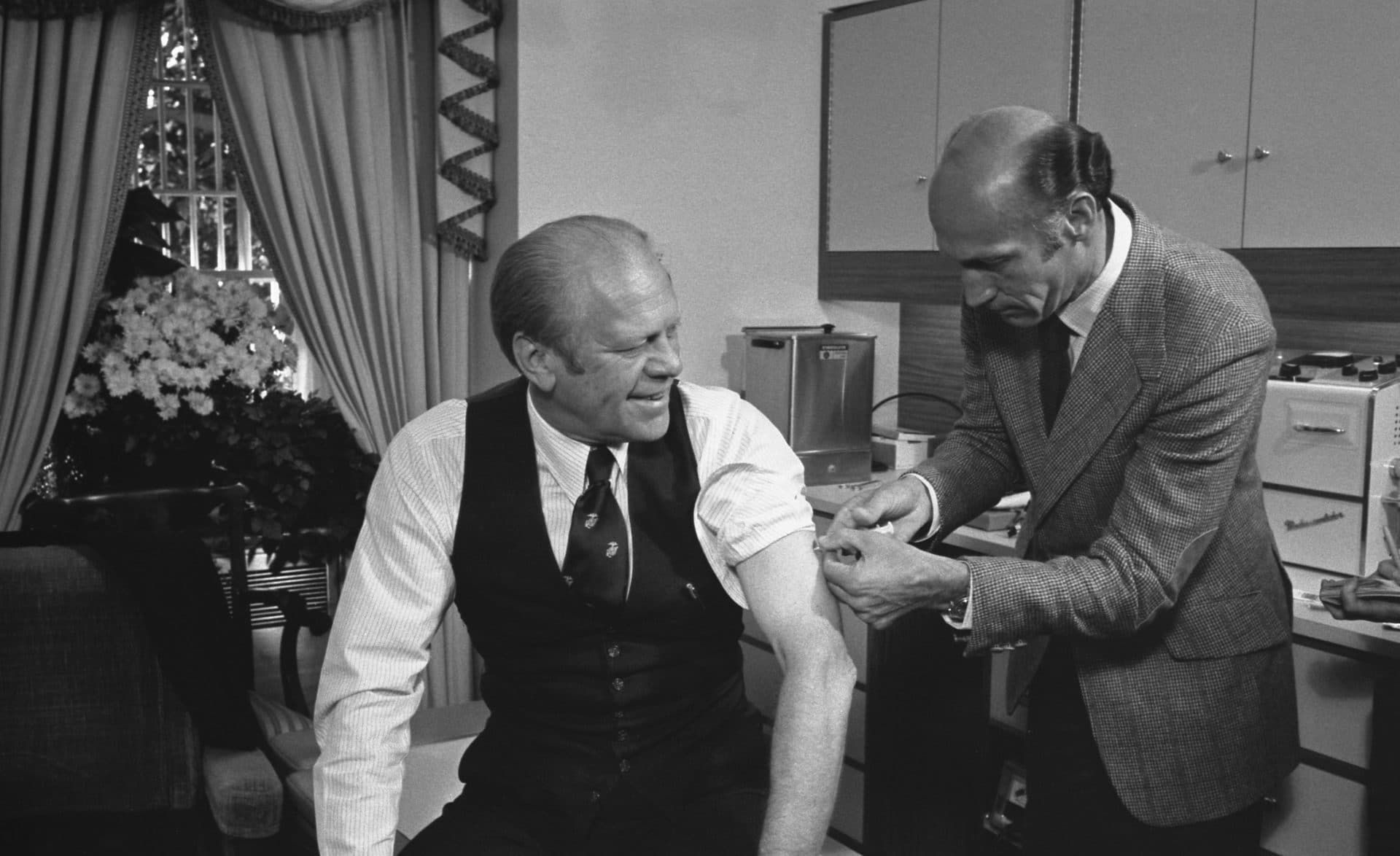
This marked the beginning of a long-term budgetary crisis that WHO still labors under. Voluntary contributions, which WHO typically can only use for the purposes designated by their donors, have accounted for an increasingly large portion of WHO’s budget pie. Up from 20 percent in the 1980s, voluntary contributions now comprise more than 75 percent of WHO’s finances. In WHO’s last bi-annual budget cycle from 2018-2019, the United States provided $650 million, or about 11 percent of WHO’s entire funding, through this type of specified contribution. The Bill and Melinda Gates Foundation was the second largest donor with contributions totaling $520 million, more than every other country. Those two voluntary contributions alone top the entirety of regularly assessed contributions ($889 million) from every single one of its 196 members.
“It never fails to amaze me that every time an outbreak happens, everyone says, ‘why is WHO not doing this or that?’” Clare Wenham, a professor of global health policy at the London School of Economics, told the Bulletin. “Well, look how much money they’ve got to do it. The whole of the WHO has less money than a mid-tier hospital in the US. And then think about how much of that is allocated to emergency response, compared to HIV, or malaria or whatever. It hasn’t got the money and the staff.”
By the early 1990s, the influenza program that had been one of WHO’s founding initiatives had dwindled dramatically. While the global influenza surveillance network stayed active sharing information about new viruses and identifying seasonal flu strains for vaccine development, by the time Cox began working at the CDC in 1988, the Global Influenza Programme employed “one senior person,” she said. “He had one other individual working with him who was responsible for putting together reports and that type of thing. They really had a very, very limited budget.”
The return of infectious disease
Despite, or perhaps because of, the lack of resources invested in pandemic preparedness, a growing chorus of expert voices began to sound alarms during the 1990s. A deadly outbreak was not a matter of if, but when, went the refrain. Security concerns at the end of the millennium turned away from Cold War fears toward new threats, and the explosive globalization of trade and air travel increased the risk of global crises. At the same time, active resurgence of epidemic diseases like cholera in South America, plague in India, and Ebola (which struck the Democratic Republic of the Congo during the World Health Assembly’s meeting in May 1995) signaled that the threats were not hypothetical—the assembly called for an update of the International Health Regulations to “ensure the maximum possible protection against infection with minimum interference in international traffic.”
Progress on the revisions was slow. But WHO’s response to the 2003 SARS coronavirus outbreak—bolstered by a new sense of urgency following the 2001 9/11 and anthrax attacks in the United States—helped push the health regulations review into high gear amid a broader securitization of health policy. China had been slow to inform WHO about SARS, waiting months before it acknowledged the outbreak and shared data. Criticism of China by WHO’s then director-general, Gro Harlem Brundtland, was seen as withering, given how uncharacteristic it was coming from the organization’s top official: “It would have been much better if the Chinese government had been more open in the early stages,” she said.
Cox, who led the CDC’s WHO Collaborating Center for Surveillance, Epidemiology and Control of Influenza from 1992 to her retirement in 2014, said the United States’ support for pandemic preparedness with WHO accelerated after the SARS outbreak and recognition of the threat posed by the H5N1, or avian flu, another virus still emerging in Asia.
“We at the CDC influenza group began getting additional designated funding for international work,” she said. “It grew significantly under the Bush administration, and it continued through the Obama administration.” She said the CDC was able to support WHO’s work on coordinating global disease surveillance by providing funding for low- and middle-income countries' own influenza surveillance networks. “We provided funding not only for some of the national influenza centers,” Cox said, “but also for keeping staff on at WHO who would be involved in looking at the data that is collected around the world and establishing platforms for data sharing and dissemination.”
That extended to working with China to improve its ability to respond to viral threats, and prevent a repeat of its first experience with the SARS coronavirus. “China now has a richer collaborating center for influenza,” Cox said. “And that was largely possible because of the collaboration that began back in 1988 through 2004—when [the CDC] actually got some funding that we could put in place—and then that collaboration really expanded from 2004 to 2020.”


International health regulation 2.0
When WHO member states finally adopted a new set of International Health Regulations in 2005, it was seen as a watershed moment for epidemic preparedness and response. The regulations expanded the classification of diseases that WHO member states were required to provide notification about—beyond cholera, yellow fever, and plague—for the first time, including influenza, coronavirus and any “unusual or unexpected” diseases.
There were other key innovations: WHO’s director-general could now declare a global health emergency (known as a Public Health Emergency of International Concern), to both signal the need for national action and trigger WHO’s authority to recommend temporary measures and guidance; WHO could now use non-state information to make emergency declarations; and the regulations obligated member states to work toward achieving core readiness to prevent and control pandemics within their own borders.
But the expanded provisions of the International Health Regulations faced their first major test in 2009, when the Swine Flu broke out. A new strain of a new H1N1 virus first was identified in Mexico in March, reaching the United States in April. Shortly afterward an IHR emergency committee convened by WHO’s then director-general Margaret Chan recommended the first declaration of an international public health emergency under the revised International Health Regulations. By June the pandemic had reached 74 countries. The CDC later estimated that in the United States, between 8,000 and 18,000 people died out of a total 60 million cases. Upwards of 200,000 likely died worldwide.
But at the time WHO was initially accused of exaggerating the severity of the pandemic, in part because a lack of transparency about the experts on the emergency committee stoked conspiracy theories that the committees members were making decisions favorable to pharmaceutical companies. A series of reports and the ultimate tally of cases eventually vindicated WHO. But the events constituted a first challenge to the usefulness of the new International Health Regulations and raised the issue of transparency about WHO’s decision-making in declaring a public health emergency or pandemic.


In 2014, an outbreak of Ebola struck West Africa, first in Guinea, then Liberia and Sierra Leone. WHO immediately deployed an unprecedentedly large contingent—more than 100 experts—via the Global Outbreak Alert and Response Network, which WHO established in 2000. But it still took nearly five more months for WHO’s then Director-General Margaret Chan to declare an international health emergency. A mid-June internal memo made explicit WHO officials’ reluctance to activate the emergency provisions of the International Health Regulations, because their use “could be seen as a hostile act in the current context and may hamper collaboration between WHO and affected countries.” As in the 19th century, the international response to public health crises remains intimately connected to concerns about trade (the West African mining industry, in this case) and politics.
Yet global health security experts say the blame cannot be shouldered by the WHO officials alone. In a 2016 assessment of WHO’s Ebola response, global health security scholar Adam Kamradt-Scott noted that just one year before the outbreak, WHO’s member states agreed to a 51 percent cut in its outbreak and crisis response budget, leaving key departments understaffed just as new epidemics were on the rise. Chan told the World Health Assembly that demands on WHO during the Ebola crisis were “more than 10 times greater than ever experienced in the almost 70-year history of this Organization.”
At the same time, WHO’s reluctance to challenge official state health reports “is arguably one of the most damning indictments of the [organization’s] performance,” Kamradt-Scott wrote. “The [WHO] secretariat’s error is made particularly acute when considering the historical record of governments’ attempts to conceal disease-related events as a result of concerns that these may lead to trade and travel sanctions—a practice that, ironically, member states had hoped would be addressed when they commissioned the IHR to be revised.”
Try, try again
In the aftermath of Ebola, WHO restructured. In 2016 Chan oversaw the launch of the Health Emergencies Programme, which centralized the agency’s work on disease and other health disasters, and established more uniformity among WHO’s three levels of governance at its headquarters and regional and country offices. Facilitating individual countries’ pandemic preparedness is a primary focus of the four-year-old program. Yet by 2019, 75 percent of WHO’s member states had still not met the requirements of the International Health Regulations.
Nevertheless, compared to the way pandemics were addressed in the 20th century, the last 20 years show an undeniable concentration of WHO’s attention to emergency response, despite the lack of funding—thanks largely to the 21st century security concerns of Western states.
In addition to recent regulation and structural reforms, new endeavors like WHO’s R&D Blueprint (which partners with researchers and the private sector to speed development of vaccines and treatments for a specific set of epidemic diseases and was among the first groups activated to begin researching measures against coronavirus) and modern surveillance mechanisms like the Epidemic Intelligence Open Source system (which first alerted WHO to the Wuhan outbreak at the end of December) have helped modernize and accelerate how WHO and the world reacts to emergent threats.
But these innovations can do little to overcome the delayed or inadequate action of member states or the funding gaps enforced by those states. By the end of 2019, the Health Emergencies Programme had only secured some 80 percent of its 2018-2019 budget. The entire funding received for the organization tasked with defending the planet against disasters like COVID-19 was $454 million—about one fifth of the 2019 New York City Fire Department budget.
Global health politics expert Kelley Lee told the Bulletin most of the efforts to improve have been insufficient to achieve real change. “I often compare WHO reforms of the past decades as rearranging deck chairs on a sinking ship,” said Lee, professor of public health at Simon Fraser University. “We are in a vicious circle—donors do not want to throw good money after bad. WHO cannot improve unless it has proper resourcing.”
“That's the problem, right?,” Wenham said. “In the inter-crisis era, people don't fund for outbreaks because it's not a political priority. It's a ‘never event’—it might not happen in your time in office. So it never gets funded.”
According to Lee and others, the confused global experience of COVID-19 is more reflective of WHO’s inherently limited capacity for enforcement than of a mandate the organization failed to meet. “It is not WHO’s responsibility to reform itself,” Lee said. “It is member states which must come together to drive change. This is where we have problems. Member states are in huge disagreement about what authority and resources WHO should be given. As a result, we are in this terrible gridlock.”
Some reports suggest that China at various points delayed notifying WHO of early cases of what came to be called COVID-19, discovery of human-to-human transmission, and the number of cases and deaths. The criticism generally follows that WHO should have known from its previous experience with SARS that China’s information was not reliable, and that WHO should have investigated further and reacted more quickly—including declaring an international health emergency sooner.
“There’s a valid debate to be had whether it took them too long to react to this,” Zimmer said. “But the idea that declaring an international public health emergency is this panacea that will cause everyone in the Western world to just focus on this and come together and get it done, it’s just not how it’s ever worked.”


At a briefing on May 6, when the global toll of COVID-19 had passed 250,000, Michael Ryan, head of the WHO Health Emergencies Programme, addressed the limitations on WHO’s ability to discover and respond to outbreaks:
“WHO has no special powers of investigation or deployment. … There are thousands of these events every year all around the world where we’re picking up signals, we seek to verify the existence of an epidemic with the country. We seek further information, but we always, on each and every occasion, offer the country assistance with investigation, diagnosis and response, and respond immediately to requests from our member states to do that. … We’ve launched in excess of 80 search team missions to support our member states already in this response. … At any one time around the world we are responding to at least 30 graded emergencies in which we have teams in the field at the request of our member states.”
Key phrase: “at the request of our member states.”
“It’s a member-state organization,” Wenham said. “When governments are like, ‘Oh, WHO is not doing anything,’ well, that’s because you didn’t give it that capacity. You didn't give it that power. You didn't give it that authority. You didn’t give it that money.
"Is it making bad decisions on its own? Or is it because it’s in a structure where it's not able to make independent decisions?”
The United States versus who?
The COVID-19 pandemic is extraordinary in its global impact. As of this writing, the global death toll exceeds half a million worldwide, with more than 130,000 in the United States. Trump and other national leaders continue to blame someone other than themselves—from China generally to WHO to governors of American states.
“It was not WHO that did not learn lessons from previous outbreaks,” Lee said, “but that member states turned to other priorities after the many reviews that followed the Ebola outbreak. The political climate over the past decade has shifted decidedly to the right, which has traditionally meant less support for multilateralism and the UN system and an increased focus on national interests.”
On July 7—as Tedros was announcing WHO's mission to China to investigate the origins of the virus—members of Congress and a UN spokesman confirmed that the White House had sent a letter officially giving notice of its intent to withdraw the United States from WHO. While Trump has shown little hesitation about cancelling hard-won treaties on arms control and discarding important environmental regulations, experts and legislators have questioned the legality of his move against WHO. The joint resolution in Congress that authorized joining WHO in 1948 requires one year's notice—well beyond the November presidential election—and full payment of US financial obligations to the organization.
As of this article’s writing, US government officials and scientists continue to cooperate with WHO on a daily basis, and there has been little, if any, explanation of how the withdrawal will work. Even less attention has been given to the fact that the International Health Regulations constitute a separate agreement that does not itself require membership in WHO, but certainly demands close cooperation with it. To truly sever all ties with WHO, would the United States have to abandon the entire body of international health rules it has observed for well over a century?
Even if Trump remains in the White House and follows through with a total withdrawal, it’s not at all clear what the move would accomplish. “Trump thinks that we’re still in the ‘80s,” Wenham said, “and the US is still the only possible superpower, and if they pull out, you know, everything’s going to come crashing down. No. It’s not. We saw China responding that they are going to put in more money into the World Health Organization. [Other countries] up their contributions to the World Health Organization, Gates ups his contribution to the World Health Organization. So the money can be filled. And the normative leadership can be filled, because quite frankly, the US administration at the moment is not demonstrating any type of leadership in terms of how to respond to an outbreak. So I think it's only going to backfire on Trump. And I don't think he’s figured that out yet.”
“Ironically, we might see less money going into global health security … if it's not led by Western actors,” Wenham said. “The whole framework of security, the whole concept of health emergencies as we talk about them now is a Western-centric concept… And the whole thing has been about preventing outbreaks from getting to the US.”
But that effort did not translate into preparedness for outbreaks once they breached US and European borders. Wenham noted the 2019 Global Health Security Index, which measured countries’ preparedness to respond to outbreaks, ranked the United States at first place overall. Of course, the United States now also ranks at the top for COVID-19 cases and deaths.
It bears remembering that epidemics affect hundreds of millions of people every year, even when the Western media don’t cover them and WHO’s member states don’t focus on them. Cholera, which was at the heart of European concerns back when international health regulation began in 1851, is estimated to infect up to 4 million people worldwide every year, killing as many as 143,000. In 2018, malaria infected 228 million people, mainly in Africa. Of the 400,000 who died, two-thirds were children under five. And HIV/AIDS has infected more than 30 million people worldwide over the last four decades.
Then there’s Ebola, which struck the Democratic Republic of the Congo (DRC) beginning in August 2018. The WHO declared a public health emergency of international concern in regard to that epidemic in July 2019. The timing and rationale for that decision was controversial, too, as the emergency committee delayed the declaration until it was unable to deny criteria like regional transmission (the virus reached Uganda in April 2019) and the potential for further international travel (after infections were identified in Goma, a densely populated transportation hub). The outbreak was declared over on June 25, after 2,287 had died. A separate, new Ebola outbreak began June 1, the eleventh in the Democratic Republic of the Congo since the virus was first detected there in 1976.
For audiences in the US, the entire episode barely registered.
“We didn't learn anything from Ebola—or rather we did learn, but we didn’t implement. How many of these reviews do we need to have before something changes? I do think from that perspective COVID is a game changer,” Wenham said. “The scale of it and where it’s affected is going to push for some sort of revision or review of the International Health Regulations in some capacity.”
Even critics of the WHO—from the red-baiting congressmen who nevertheless voted for it in 1948, to Reagan in the 1980s, to the many experts today who share concerns about future pandemics—ultimately acknowledge that if something like WHO did not exist, the world would have to invent it. What its inventors choose to do with it is the question.
“It’s not up to WHO officials to make us care about something,” Zimmer said. “Right?”









Terrific article and I will push for my country, Canada, to give money without strings attached. I am one citizen, but that’s how it starts. I belong to the New Democratic Party of Canada and will start by raising it there.