Keep your mask on: Why a coronavirus vaccine won’t be the panacea many hope for
By Eileen Choffnes | September 30, 2020
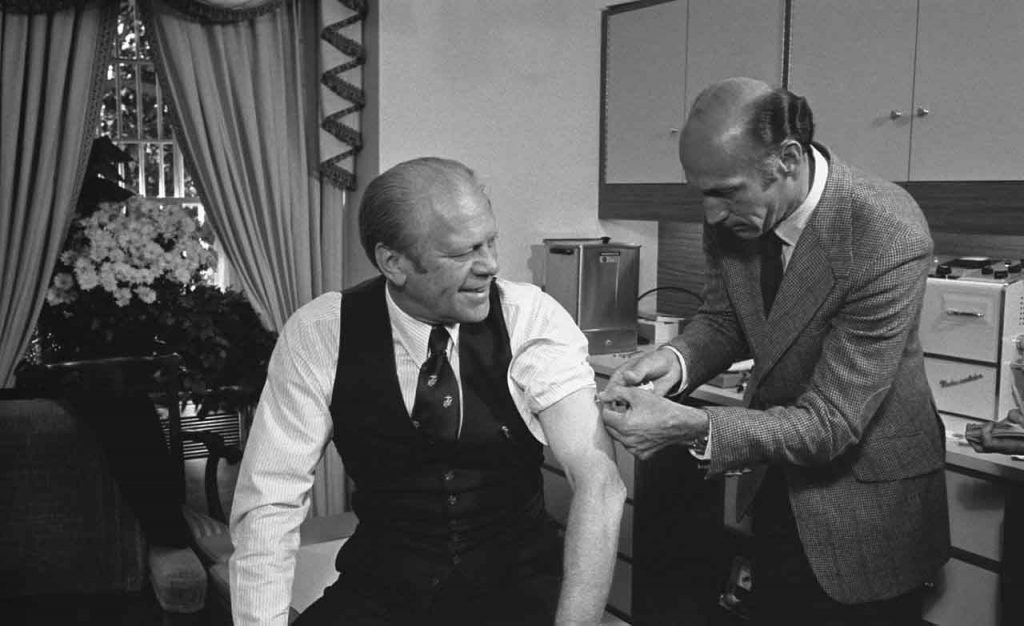 Facing the threat of a swine flu pandemic, President Gerald Ford's administration vaccinated more than 40 million people in 1976. The pandemic never materialized, and the program was linked to unexpected rates of Guillain-Barré Syndrome, a neurological condition. Credit: David Hume Kennerly/Gerald R. Ford Presidential Library via Wikimedia Commons.
Facing the threat of a swine flu pandemic, President Gerald Ford's administration vaccinated more than 40 million people in 1976. The pandemic never materialized, and the program was linked to unexpected rates of Guillain-Barré Syndrome, a neurological condition. Credit: David Hume Kennerly/Gerald R. Ford Presidential Library via Wikimedia Commons.
Last week, we learned the United States had finally passed a threshold that at one time might have seemed unimaginable, 200,000 deaths from COVID-19. We passed this grim milestone despite months of lockdowns, PSAs about social distancing, mask wearing, and other interventions to slow the spread of the SARS-CoV-2 virus. If low-tech measures have not worked well in the United States to stop COVID-19, what will? Many hope the global race to develop a vaccine against the novel coronavirus will bear fruit. The theory goes something like this: We will have a vaccine against the coronavirus; nearly everyone will want to be vaccinated; and, afterward, we can return to the way things were before COVID-19 became part of our lives. We can stop holding our breath, exhale, throw away our masks, and go back to living our lives.
But that’s not likely to happen anytime soon.
Since the 18th century vaccines have been enormously influential in saving millions from the death and illness associated with infectious diseases. In some cases, vaccines have totally eradicated these illnesses, including smallpox in humans and rinderpest in cattle. In other cases, childhood immunizations, such as those for mumps, measles, diphtheria, and rubella, have made getting sick or dying from once common diseases largely a thing of the past. That’s why we are eagerly awaiting a vaccine against COVID-19.
Vaccine development normally costs hundreds of millions of dollars and can extend over a decade while a vaccine candidate goes through a series of four stages of testing: from pre-clinical to clinical trials. Under normal circumstances, after up to five years of basic research into the immune response and an additional two years of animal testing, vaccine candidates begin moving through phase 1, 2, and 3 human clinical trials. Trials can involve tens of thousands of people and are used to establish the safety and effectiveness of the vaccine candidate.
Even after a vaccine candidate receives regulatory approval, it still must be manufactured at scale and delivered to the target population without losing potency (some vaccines require cold storage at minus 70 degrees Celsius). Health practitioners need to be trained to properly administer the vaccine. While President Donald Trump and government health experts have given conflicting timelines, the consensus view is that a vaccine won’t be widely available until sometime in 2021.
While many of us want a COVID-19 vaccine developed and distributed as quickly as possible, at least as important as a quick process is strong regulatory oversight that ensures vaccine development follows sound science and is not influenced by political considerations.
The annals of vaccine history are full of cautionary tales.
In 1955, at a time when summer polio outbreaks led to thousands of infections, the government announced the first vaccine against polio, a disease which—in the worst cases—can cause paralysis or even death. It affects mainly children, and by 1955 was a cause of profound fear in the United States. But a company that made the vaccine, Cutter Laboratories, failed to properly inactivate the virus before it was administered to 200,000 children; 40,000 kids contracted abortive polio, 200 were paralyzed, and 10 died. In the fallout from the Cutter Incident, as it’s known, the government strengthened regulatory oversight of vaccines.
In a case of hasty decision-making during an election year, epidemiologists at the Centers for Disease Control and Prevention predicted early in 1976 that an H1N1 swine flu influenza virus would cause a pandemic. They convinced the Ford Administration to prepare a vaccine against it. In late March, President Gerald Ford announced his goal of immunizing the entire population. Seven months later, the government began vaccinating more than 40 million people.
Several hundred people contracted a rare neurological condition—Guillain-Barré Syndrome—after being vaccinated. While the syndrome is naturally occurring, a debate raged at the time about whether the cases could be directly linked to the vaccination program. According to a history of the vaccination campaign published in the Centers for Disease Control and Prevention’s journal Emerging Infectious Diseases, the consensus view of epidemiologists was that cases were in excess of what would normally be expected. The program was suspended in mid-December. On top of that, the feared swine flu epidemic never materialized, and the Ford administration’s immunization campaign may have contributed to Jimmy Carter being elected president in 1976.
Problems can crop up even after clinical testing of a vaccine. In 1998, RotaShield, a rotavirus vaccine manufactured by Wyeth, was licensed for use in the United States. Clinical trials in the United States, Finland, and Venezuela had found it to be 80-to-100 percent effective at preventing severe diarrhea caused by a strain of rotavirus, and researchers had detected no statistically significant serious adverse effects. One year later, Wyeth withdrew it from the market after it was discovered that the vaccine may have contributed to an increased risk for bowel obstruction in 1 out of every 10,000 vaccinated infants. There was a seven-year hiatus until rival manufacturers were able to introduce new vaccines against rotavirus that were safer and more effective.
Some researchers worry that COVID-19 vaccine trials are not designed to run long enough to determine whether vaccine candidates will be effective at achieving their most important goal: preventing serious illness.
In a recent opinion piece in The New York Times, Eric Topol, a professor of molecular medicine, and Peter Doshi, a professor and medical journal editor, analyzed the recently published trial protocols for three leading candidate vaccines produced by Moderna, Pfizer, and AstraZeneca. They argue that the trials may prove only that the vaccines ward off mild COVID-19. For a trial participant to be counted as sick, a cough and a positive test will suffice under Moderna and Pfizer’s protocol, and mild symptoms plus a fever under AstraZeneca’s. The trials won’t establish that the vaccines protect against moderate or severe disease, or that they lower the risk of hospitalization, admission to the intensive care unit, and death. “To say a vaccine works should mean that most people no longer run the risk of getting seriously sick,” the authors wrote. “That’s not what these trials will determine.”
According to a report in The Washington Post, the Food and Drug Administration may require vaccine makers to find at least a handful of severe COVID-19 cases among the clinical trial participants who receive the placebo treatment as well as to follow participants for two months after they receive their second vaccine injection.
As Topol and Doshi argue, giving a vaccine to hundreds of millions of people that has only been tested on tens of thousands for a short period of time, “requires a real leap of faith.” Children, adolescents, and pregnant women have been excluded from these trials; while those with pre-existing conditions, the elderly, Blacks, Hispanics, and Native Americans may be underrepresented in some late-stage clinical trials.
From the armed protestors who stood on state house steps demanding an end to pandemic lockdowns to altercations over mask wearing, the United States’s pandemic response has been highly politicized. Trump’s insistence that a vaccine will be available before the November 3 election has, for obvious reasons, only exacerbated those concerns. So has his perceived meddling in the Food and Drug Administration’s regulatory process for coronavirus therapeutics such as hydroxychloroquine and convalescent plasma that lacked strong scientific evidence to support their use.
Politicization of a COVID-19 vaccine could lead to even greater vaccine skepticism in the United States—to say nothing about what could happen if a flawed vaccine were approved for political expediency.
Even if a vaccine is found to be safe and effective, even if the government is able to get it distributed efficiently, it still won’t necessarily be the panacea many people hope for. Enough people need to get vaccinated to either prevent an epidemic or stop an ongoing one. Many in the United States are already wary of vaccines, and the so-called anti-vax movement has been growing for years. In 2018, only one in three people received the seasonal influenza vaccine. If there’s such low demand for a COVID-19 vaccine, the prospects for quashing the pandemic through inoculation could be dim.
A team of investigators lead by Bruce Y. Lee demonstrated in a computer modelling study that if 75 percent of the population gets vaccinated, the vaccine needs to be 70 percent effective in order to prevent an epidemic and at least 80 percent effective to extinguish an ongoing one. The thresholds are even higher if just 60 percent of the population gets vaccinated: the vaccine must be 80 percent effective to prevent an epidemic and 100 percent effective to extinguish one.
The Food and Drug Administration’s current threshold for COVID-19 vaccine approval is an efficacy of 50 percent, which is a pretty low bar. Even if 100 percent of the population of the United States received a vaccine that was 50 percent effective, we might not achieve vaccine-induced herd immunity.
Despite the growing enthusiasm from some about the COVID-19 vaccine trials, and the pre-ordering of hundreds of millions of units of vaccines from manufacturers whose products have yet to establish their safety and efficacy, a COVID-19 vaccine is unlikely to be the magic bullet that ends the pandemic.
A vaccine against COVID-19, once one becomes available, is only one tool in a tool box of collective and individual actions that will need to be taken to bring the spread of the virus under control. According to Anthony Fauci, the head of the National Institute of Allergy and Infectious Diseases, the United States should not expect a return to normal until “well into 2021, maybe even towards the end of 2021.”
Robert Redfield, the Director of the Centers for Disease Control and Prevention, appeared to try and lower expectations in a vaccine and to boost low-tech interventions during a recent congressional hearing. “If I don’t get an immune response, the vaccine is not going to protect me,” he said. “This face mask will.”
So how do we control this pandemic while we are waiting to exhale? Through the rigorous application of low-tech practices like mask wearing; COVID-19 testing of symptomatic and asymptomatic people (with results available within hours instead of days); contact tracing for positives cases; physical distancing; and hand hygiene. While not “sexy” these measures worked a century ago during the Spanish Flu pandemic to control the spread of disease in the United States and elsewhere, and they can work again during this pandemic.
Together, we make the world safer.
The Bulletin elevates expert voices above the noise. But as an independent nonprofit organization, our operations depend on the support of readers like you. Help us continue to deliver quality journalism that holds leaders accountable. Your support of our work at any level is important. In return, we promise our coverage will be understandable, influential, vigilant, solution-oriented, and fair-minded. Together we can make a difference.
Keywords: 1976 swine flu, Coronavirus, Operation Warp Speed, polio, rotavirus, vaccine
Topics: Biosecurity














Given the history of the flu vaccine and that 40,000 people die in an average year from the flu, betting on a vaccine to stop this pandemic is likely to be a losing bet. Some day we will get serious about air-borne pandemics—at which time we will get serious about engineering solutions. Water-borne pandemics were stopped by the engineering solutions of clean water and sewer that destroyed the environmental niche (dirty water) that spread disease. Food poisoning was stopped by sterilization and refrigeration. Medical strategies became effective backups to the front-line engineering solutions.. Air-borne pandemics can be stopped by engineering… Read more »